Review of Treatment Goals
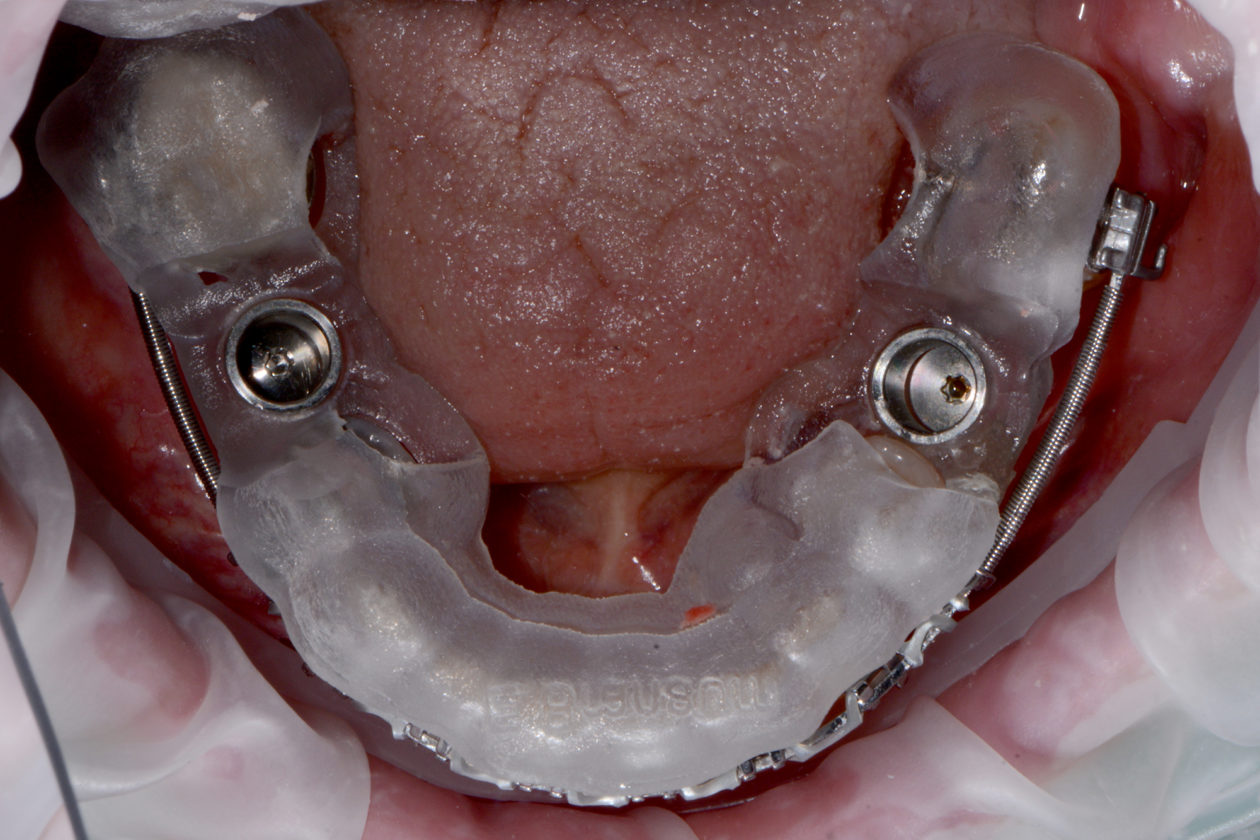
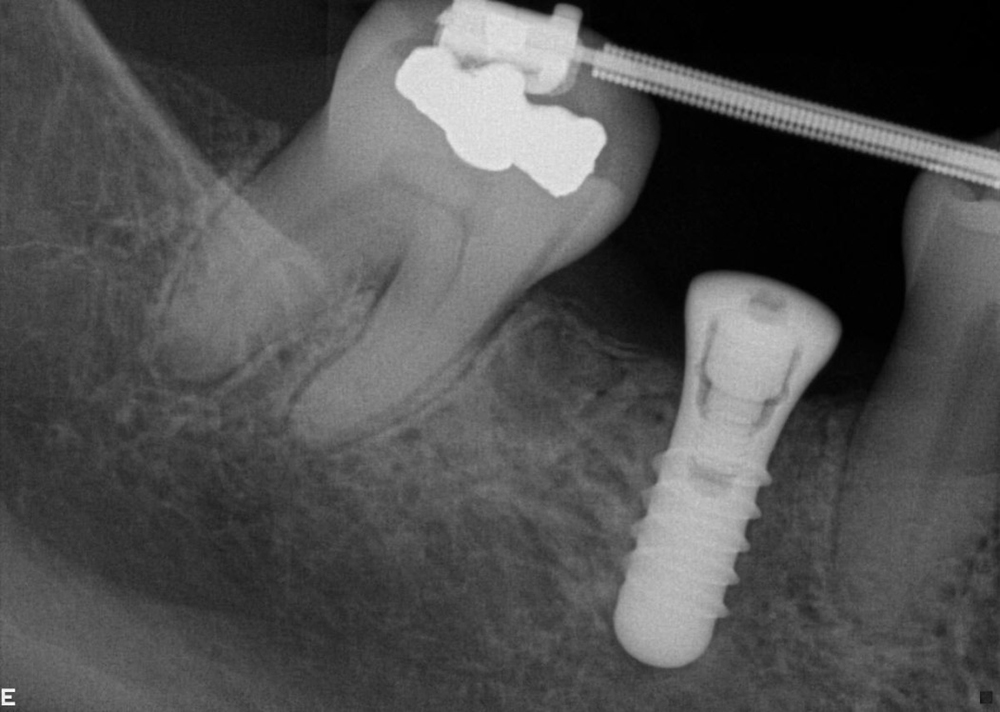
Our non-clinical goals in this case were to convey to the patient that her problems were an interdisciplinary, complex issue that had been ongoing and worsening for many years. Our solution to these problems would require the collaborative efforts of a team of dentists. The objective clinical goals were to orthodontically move her teeth into a less restrictive position and create room for restoration of lost tooth structure. Implants would be used not only to replace missing teeth but to provide orthodontic anchorage to facilitate movements that would not be possible with conventional orthodontics. Our final restorative goals were to reestablish ideal form and function, creating an occlusion that was stable and comfortable, enabling long term dental health. As her desires were specifically not to address esthetics, we were clear esthetic improvements were the result of correcting form and function. Of note is the fact that this case, from the restorative and surgical standpoint, was to be accomplished, with few small exceptions, entirely digitally.
Phase I: Initial ‘Emergency’ Treatment
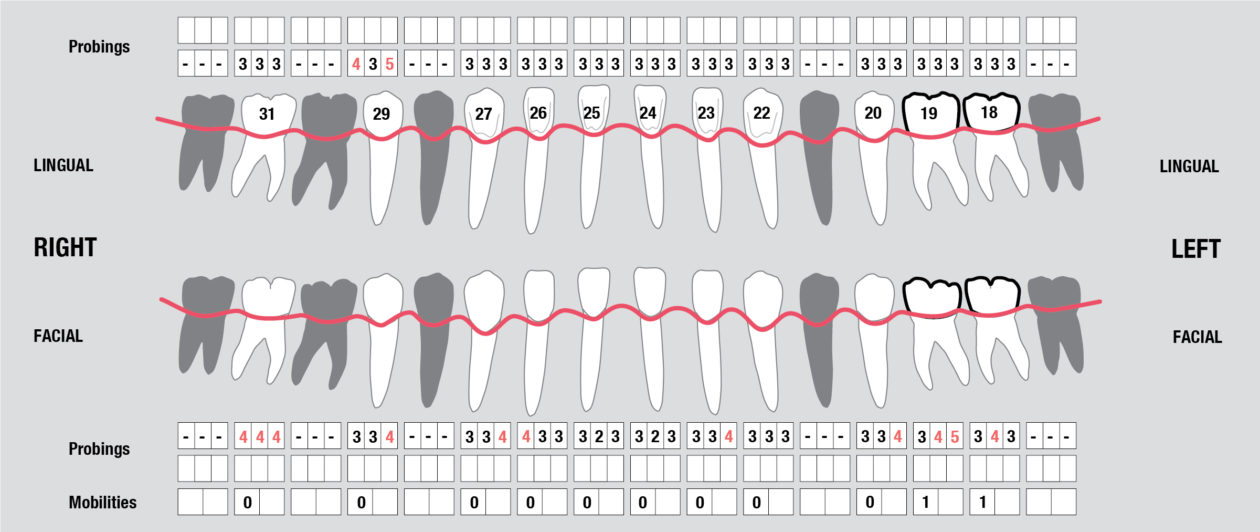
Tooth no. 19 was isolated with a dental dam under local anesthesia. All existing restorative material and decay was excavated leaving a very evident crack into the pulp, down to the pulpal floor. The mesial canals were completely calcified, the decay extended beyond the bone level. This tooth was diagnosed as hopeless and scheduled for removal. A provisional was placed at this appointment.
Tooth no. 30 was deemed hopeless at initial evaluation and extracted.
Phase II: Diagnostic Data Accumulation and Treatment Planning
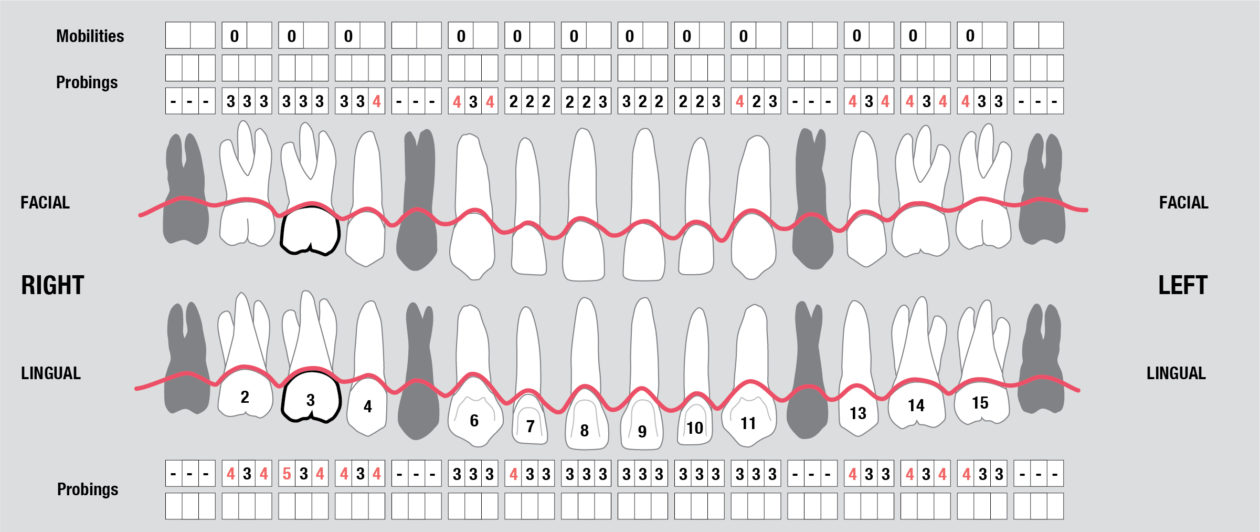
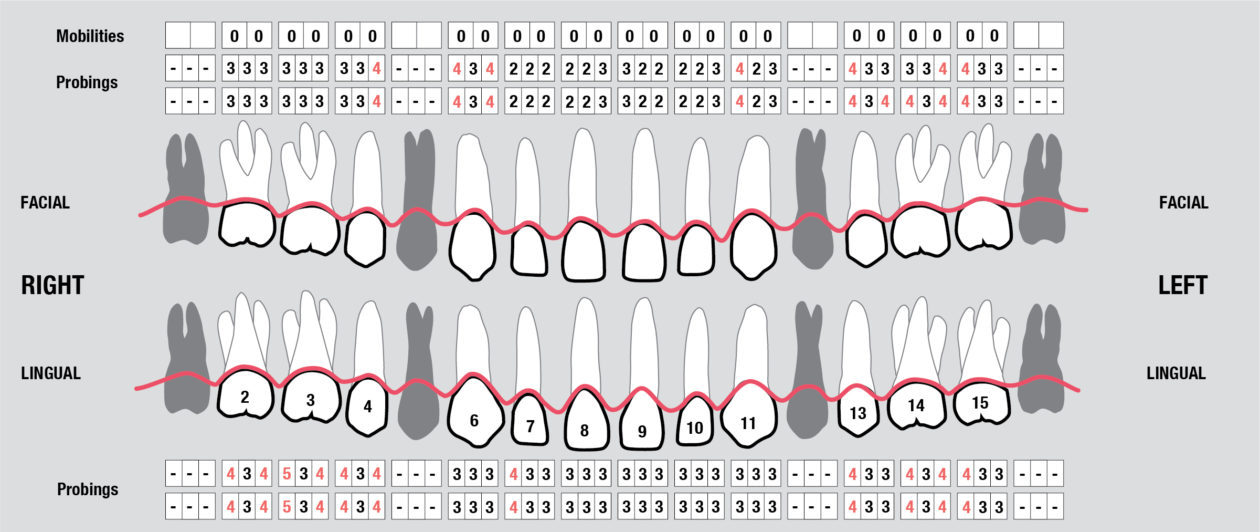
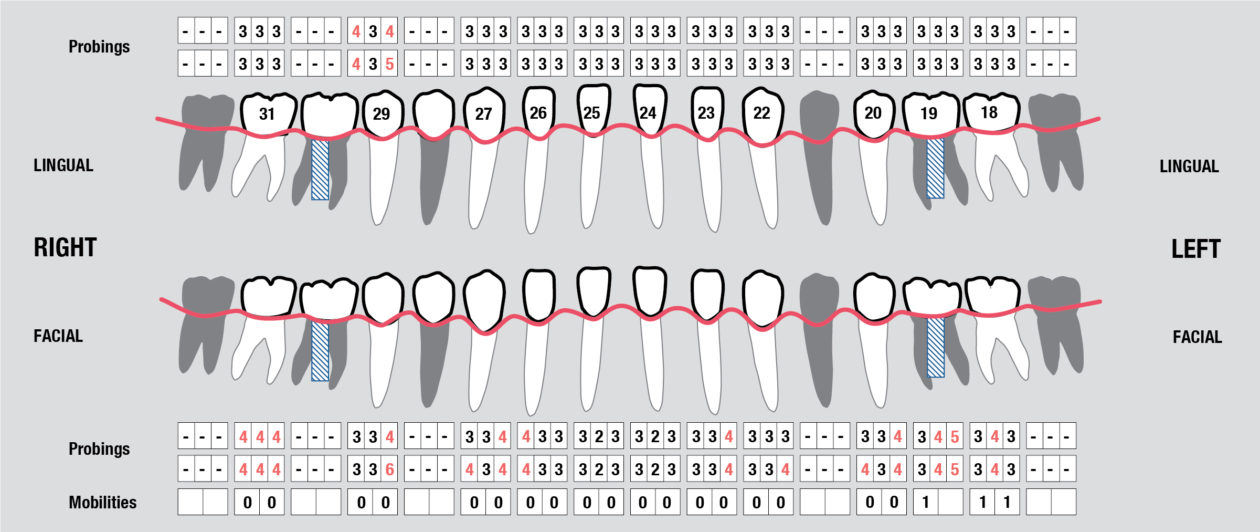
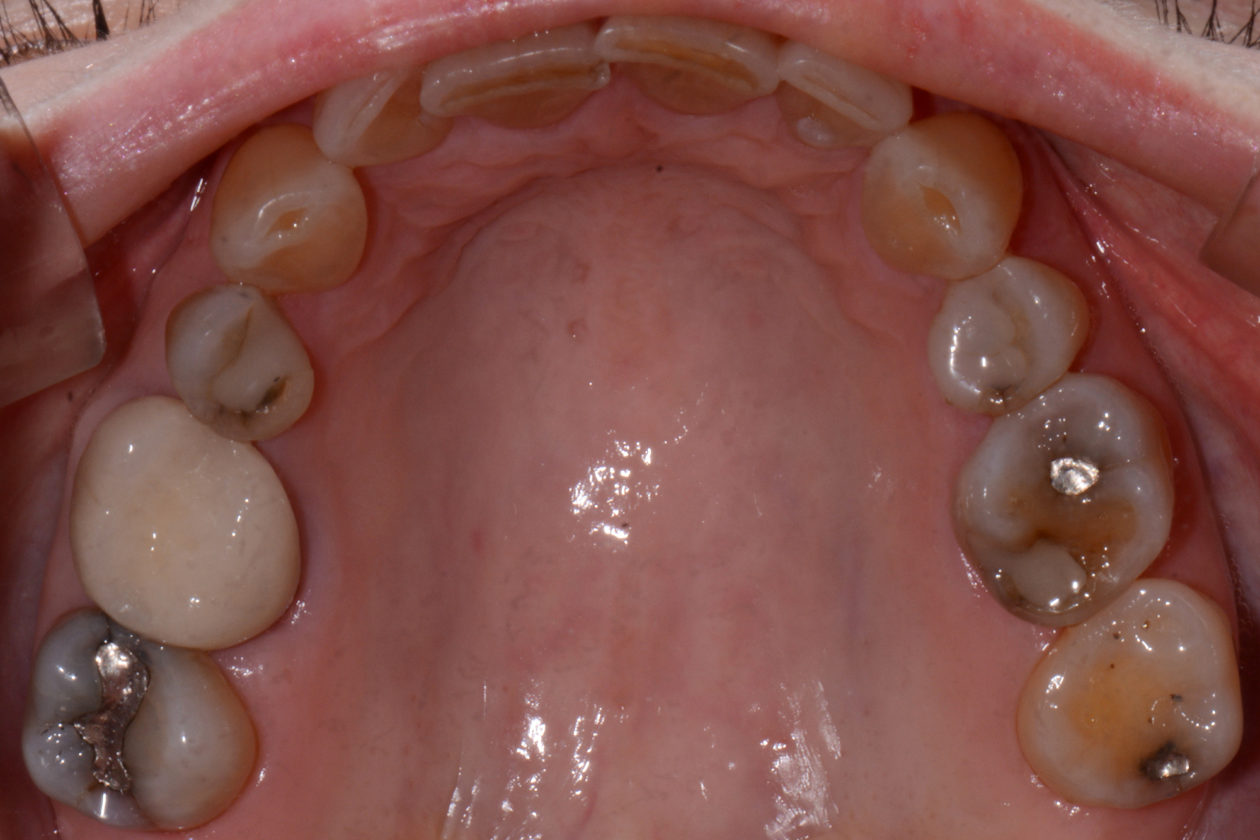
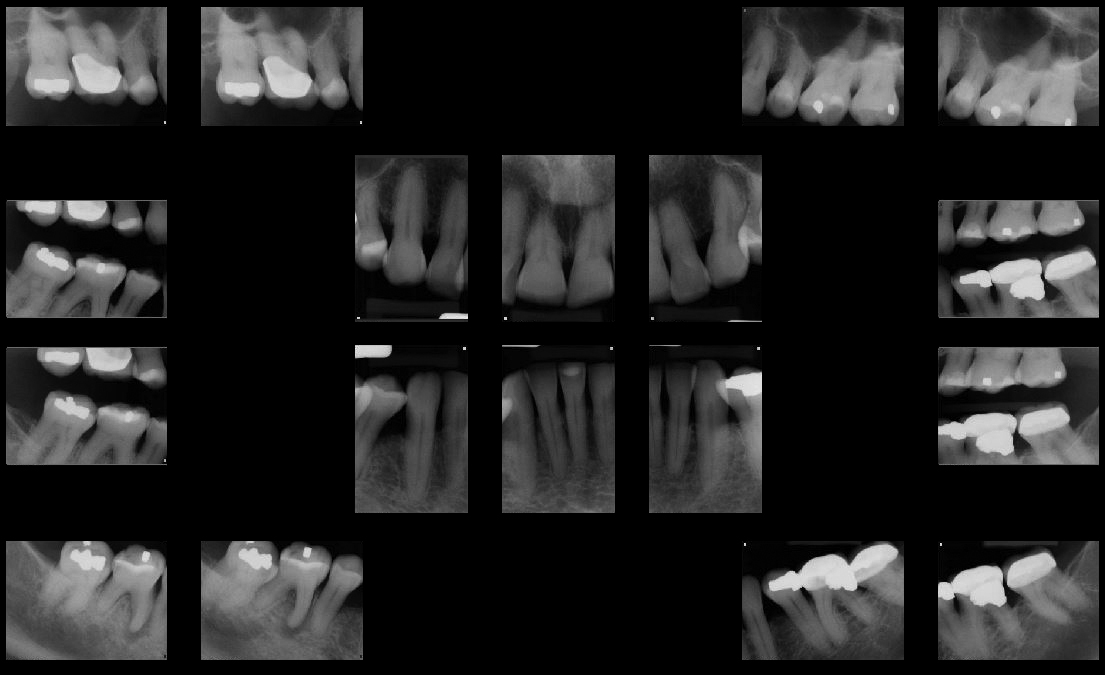
Full Mouth Radiographic Series, Maxillary and Mandibular Intraoral Scans, Digital Jaw Relation Recording with a Leaf Gauge, Complete Photographic Series, Periodontal Charting, Restorative Charting.
Phase III: Treatment Planning Consultation and Treatment Presentation
In considering a treatment plan for our patient, it is important to note that in our initial information gathering she was clear she had no esthetic concerns. Further, her desires were single tooth in nature, specifically to replace her missing lower molar teeth. The most challenging aspect of this plan was communicating to the patient what her true problem was and having her accept that the problem, if left untreated, was a challenge to her dental health for life. She must also understand the solution to the problem and to appreciate that comprehensive care with orthodontics and restorative dentistry is to solve a long standing functional and structural problem. Esthetic improvements are a consequence of restorative and structural improvements, not a primary driver in the plan. In our multiple consultation appointments, we allowed the patient to ask as many questions as she needed answered. In short, it took her about six months to overcome the single tooth mindset that she had been taught by her previous dental experiences. Photographs were a significant component in our explanation. They demonstrated the excessive wear resulting in the extractions and were an indicator of what she should expect if she chose only to have the missing lower molars replaced. The orthodontic consultation was a key in her accepting care. An opinion from one of our specialist colleagues, another set of eyes if you will, added support for our recommendations. The plan ultimately accepted by the patient was altered from our originally proposed plan per the patient’s request to only restore the mandibular posterior teeth leaving the mandibular anterior teeth unrestored. With this compromise we still felt we could achieve acceptable anterior function. That altered our overall plan in two ways. First, the orthodontic plan would now not include intrusion of the lower anterior teeth as the incisal edges will dictate tooth position, not the gingival levels. The orthodontist would place the incisal edges of these teeth in ideal position. And second, when restoring the mandibular posteriors after placement of the maxillary restorations, we will not alter the VDO.
Phase IV: Periodontal Surgery Therapy
Connective tissue grafting was accomplished pre orthodontically to cover the root surfaces in teeth nos. 11 and 12.