The agenesis of maxillary lateral incisors is a common developmental anomaly which presents an orthodontic and prosthetic challenge that often requires interdisciplinary collaboration for an ideal treatment result. The two most common treatment approaches in these cases are space opening for prosthetic restorations and space closure with the use of permanent canines as substitutes for the missing teeth. In order to meet both esthetic and functional goals, selection of the most appropriate treatment plan requires consideration of the patient’s malocclusion, growth pattern, facial profile and smile line, along with the size, shape and color of the canines.
If future placement of single tooth implants is recommended in young patients, special care must be taken because implants cannot be placed until facial growth is complete. The late Dr Vince Kokich suggested that in these cases, the lack of eruption of permanent lateral incisors prevents full development of the osseous ridge needed to place implants. As such, he recommended extraction of the primary lateral incisors in order to encourage eruption of the permanent canines next to the central incisors. He then recommended orthodontic distalization of the canines into their ideal positions in order to allow for the development of the buccolingual width needed for future implant placement.
In this case study, we present an alternative approach for the successful maintenance of both vertical and buccolingual bone dimension for future implant placement in a growing patient. Given that bone augmentation tends to be less predictable in the vertical dimension than in the horizontal, it is our opinion that maintenance of vertical bone level is more critical in cases where single tooth implants are planned. Maintenance of vertical bone is particularly important in these cases because its loss can present a cosmetic challenge, especially when patients have high smile lines.
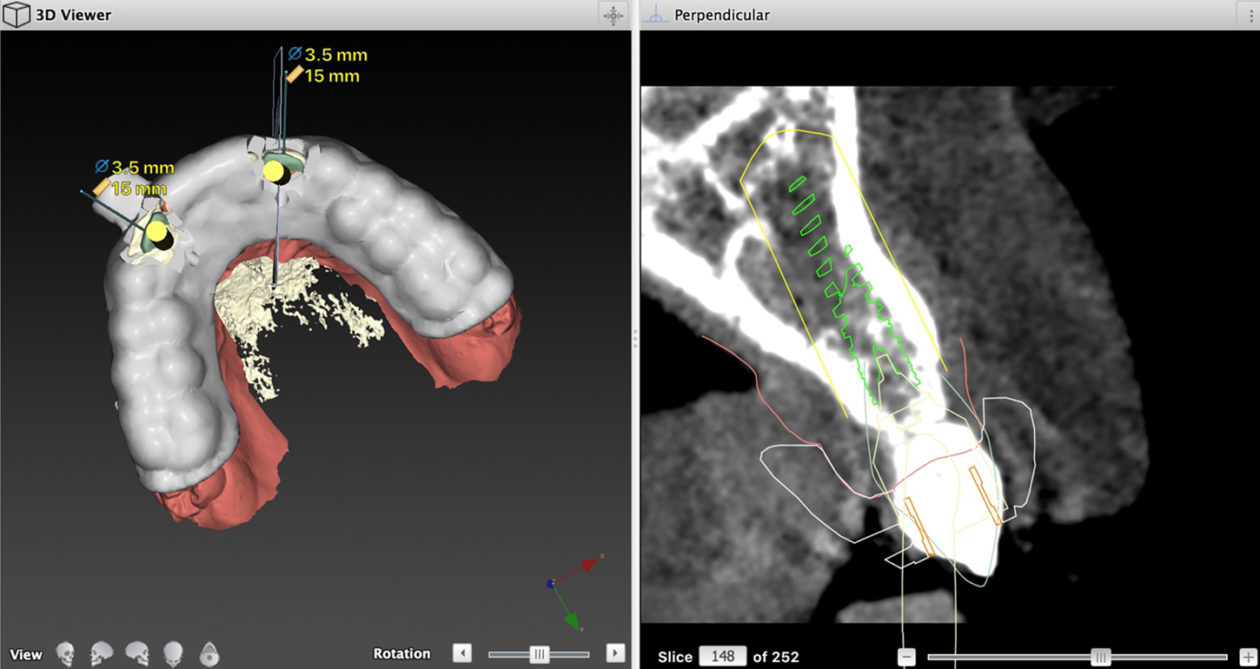
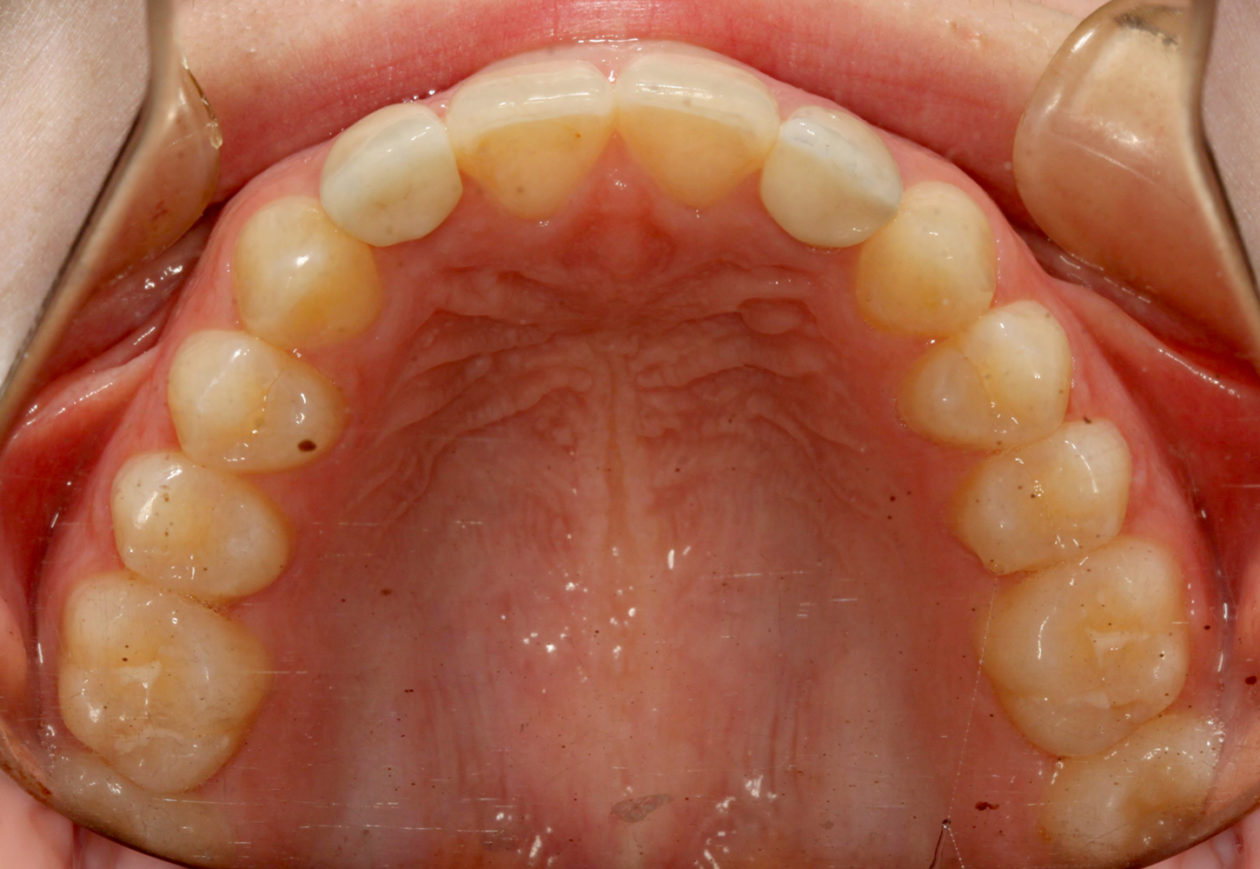
By illustrating a case in which primary maxillary lateral incisors are maintained in a patient whose permanent maxillary laterals are missing, we show successful preservation of both vertical and buccolingual bone dimension during and after orthodontic treatment. We then demonstrate successful placement of single tooth implants without the need for bone augmentation after the completion of growth.