Case 103: Save or extract? – A Case Quandry in Meeting Functional and Esthetic Needs
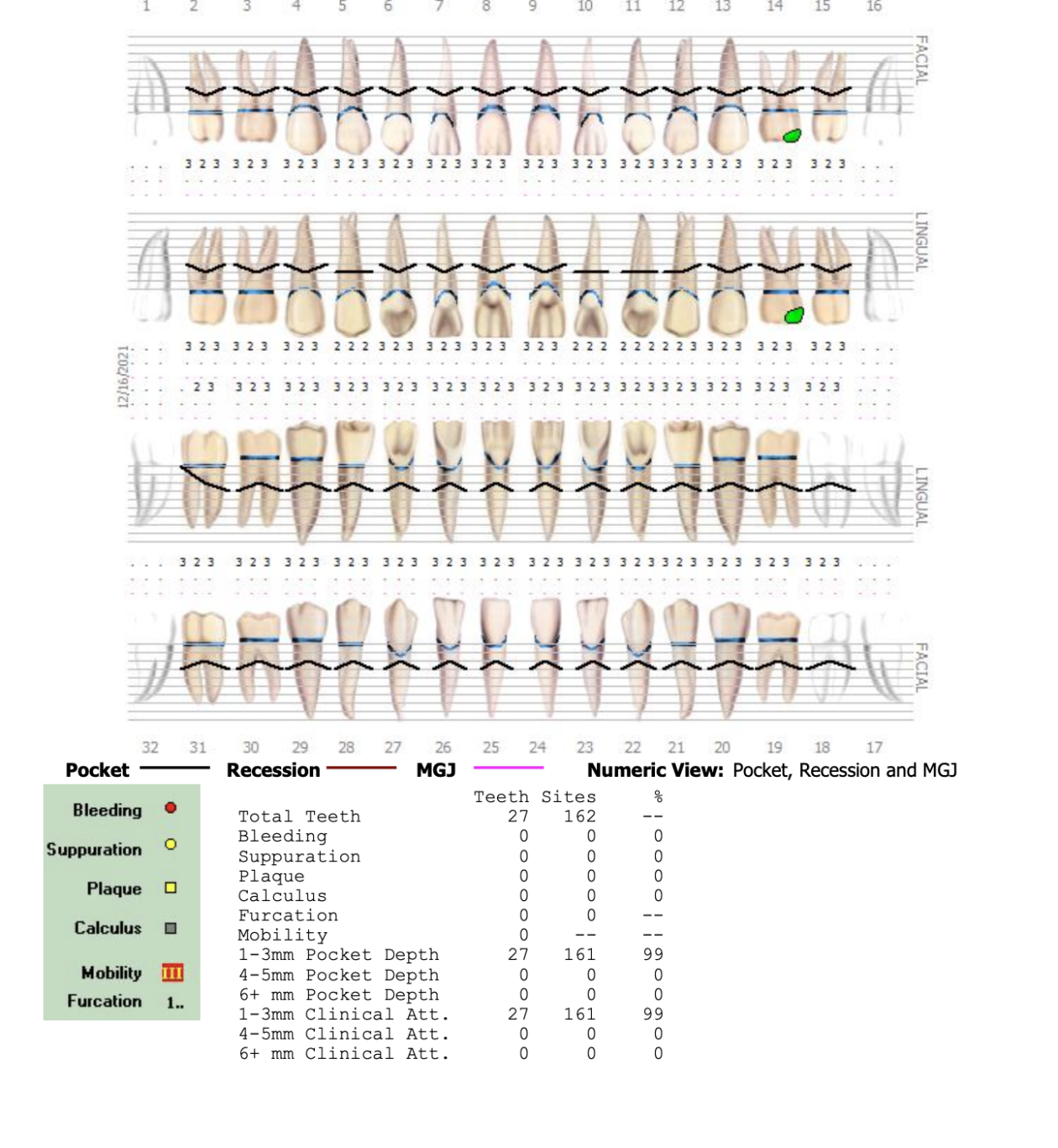
The patient presented to our office seeking a 2nd opinion for treatment options related to treating a deteriorating dentition. She also had concerns about her smile and the appearance of her teeth. She was acutely aware of her asymmetric smile and felt that she looked far older than her age (Fig 1).
Her previous dentist had recommended full-mouth extractions, followed by an implant-supported prosthesis. Although she was willing to accept this, she did not want to lose her natural teeth, if possible.
The patient also had functional concerns. She did not have a comfortable "home" position and was aware of grinding her teeth during the day. There was an extreme loss of tooth structure, and yet she was only experiencing some moderate tooth sensitivity.
During the initial interview, the patient expressed concern about the potential financial burden but seemed committed to finding a way to manage treatment.