Extraction of teeth nos. 4, 6, 8, 9, 11, 12 and 14 was completed.
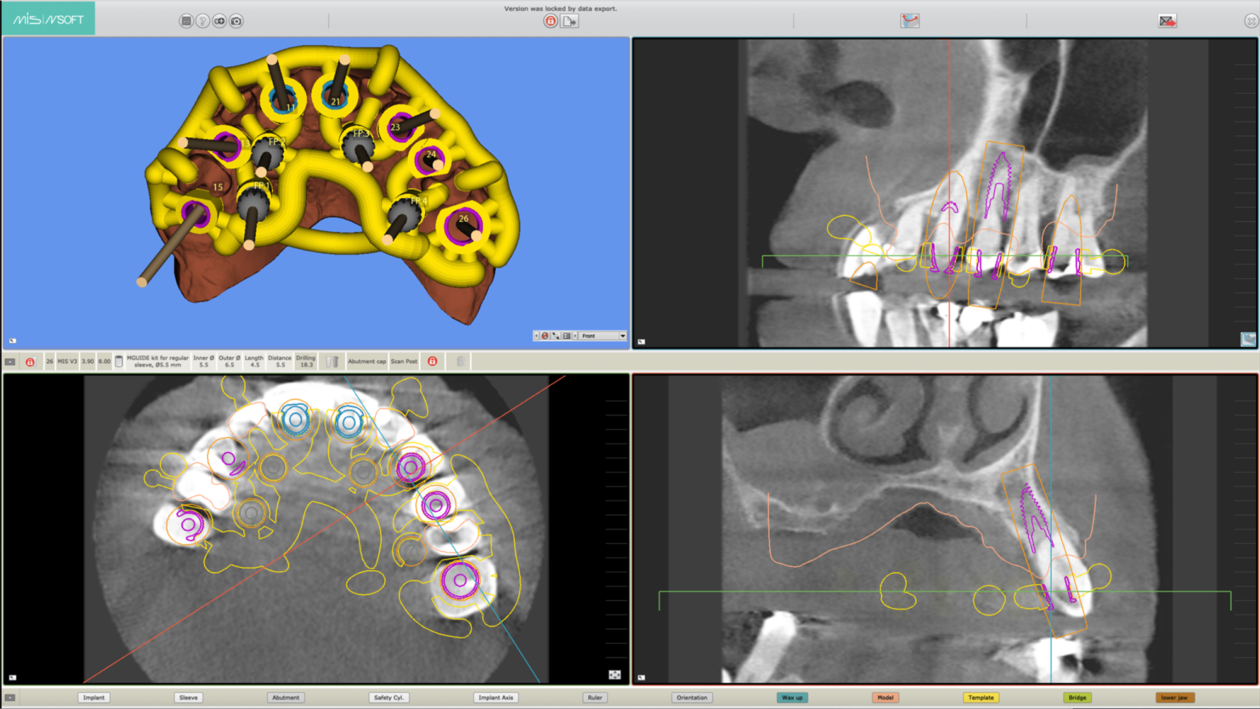
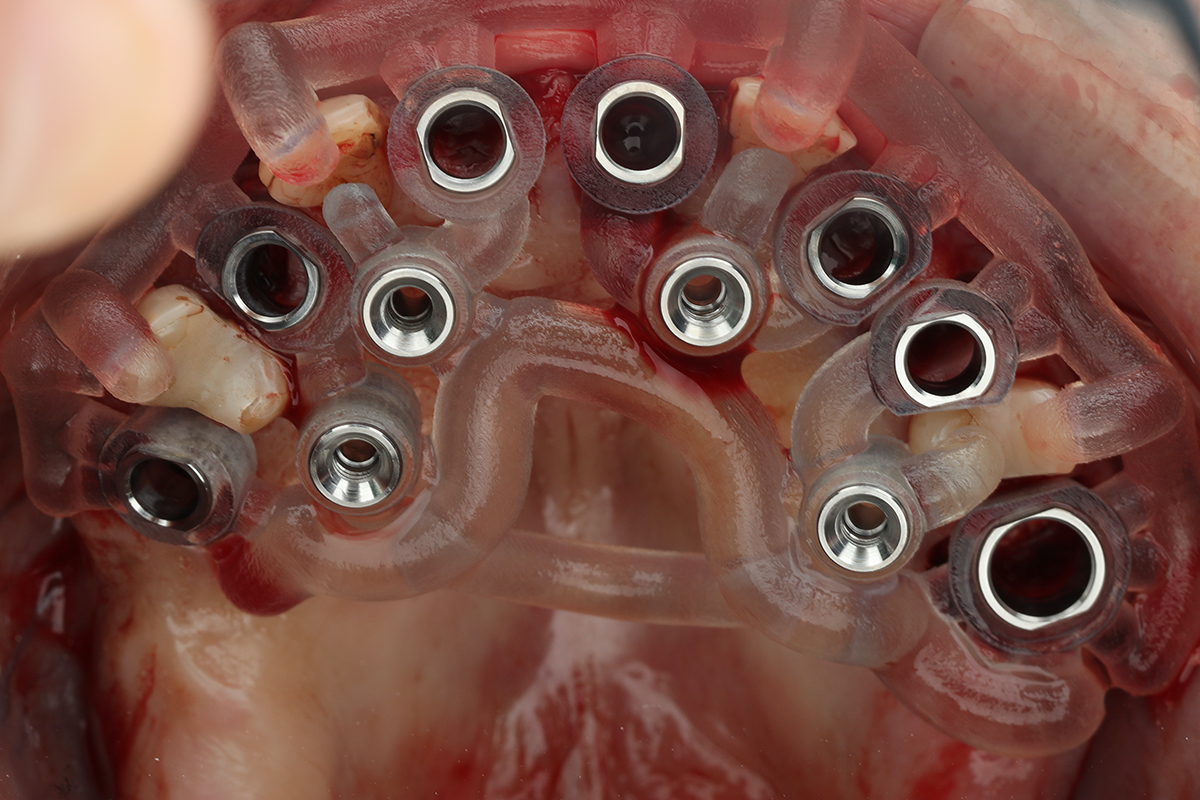
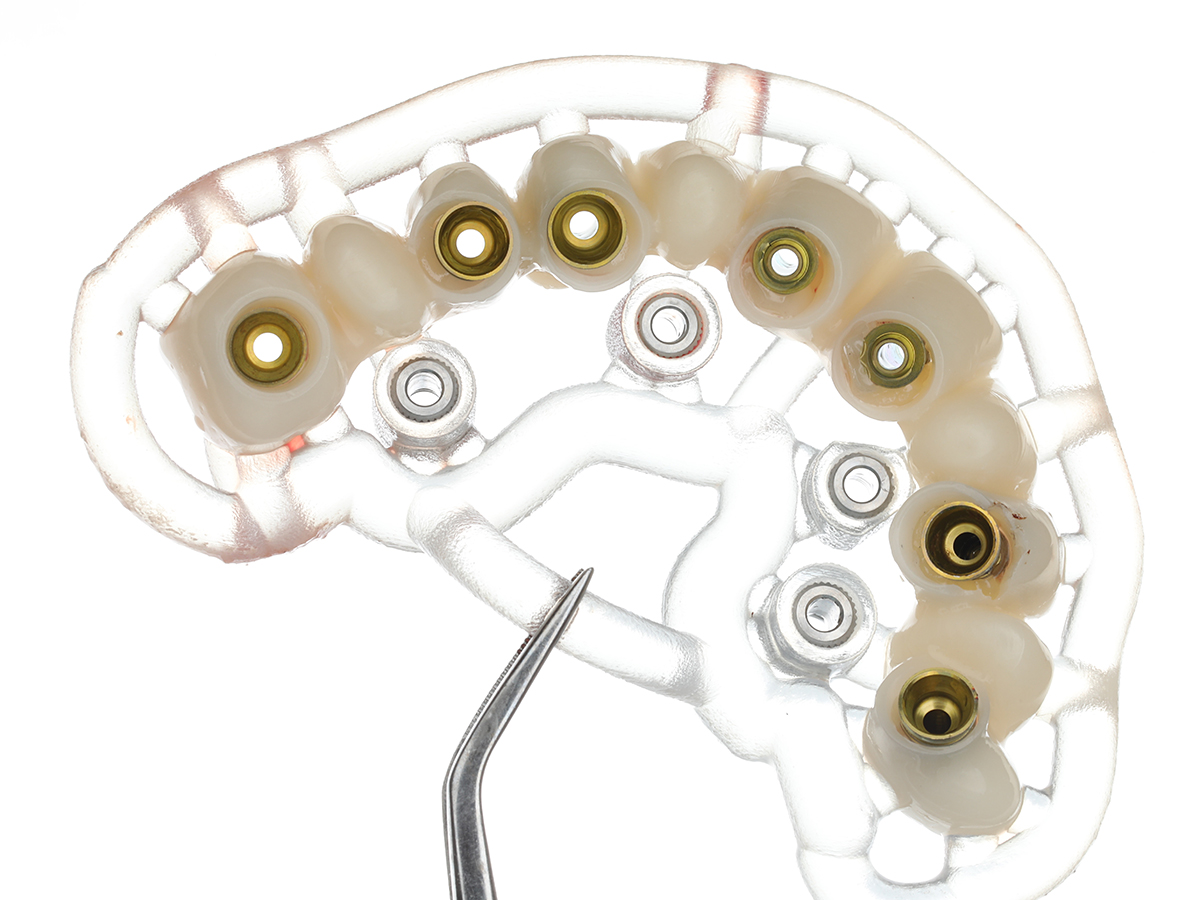
The implant surgical guide was secured onto the remaining teeth and the fit was verified. Afterward, implant site osteotomies were created using sequential drills, followed by fully guided implant placement (MGUIDE, MIS Implants, Bar Lev, Israel) protocol. In total, seven implants were placed in the maxilla. (V3, MIS Implants, Bar Lev, Israel)
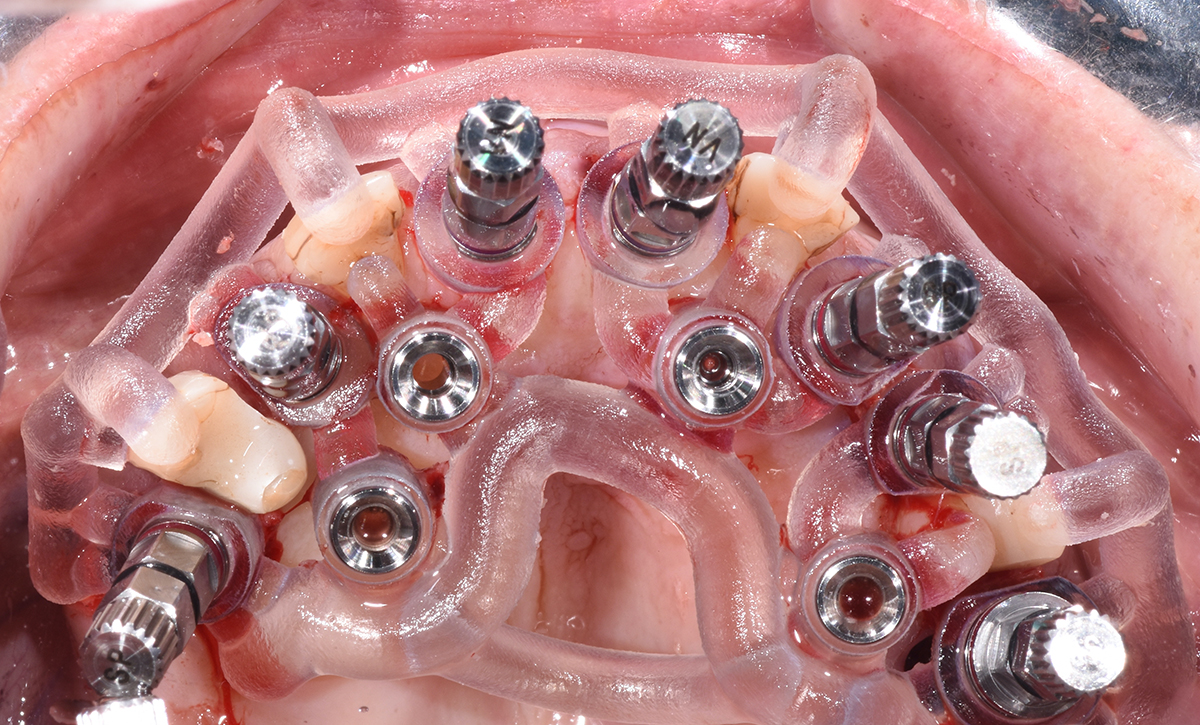
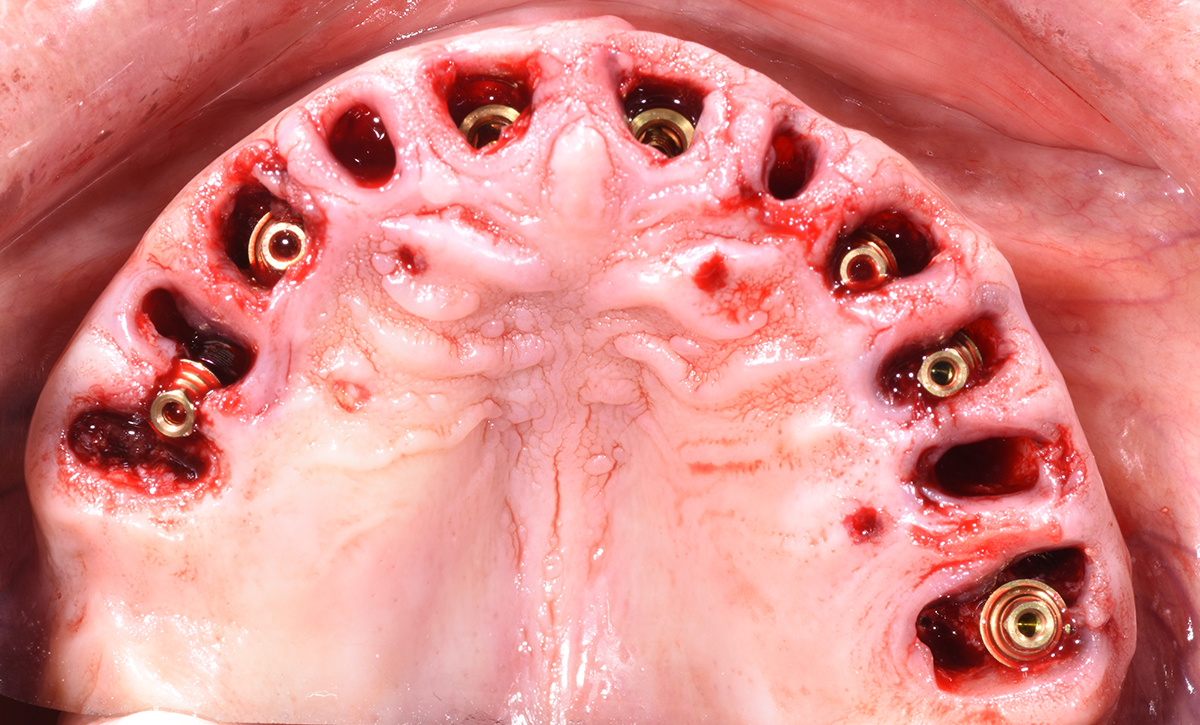
After all implants were installed, drilling of the anchor pins took place. Then the surgical guide was removed and the remaining teeth nos. 5, 7, 10 and 13 were extracted.
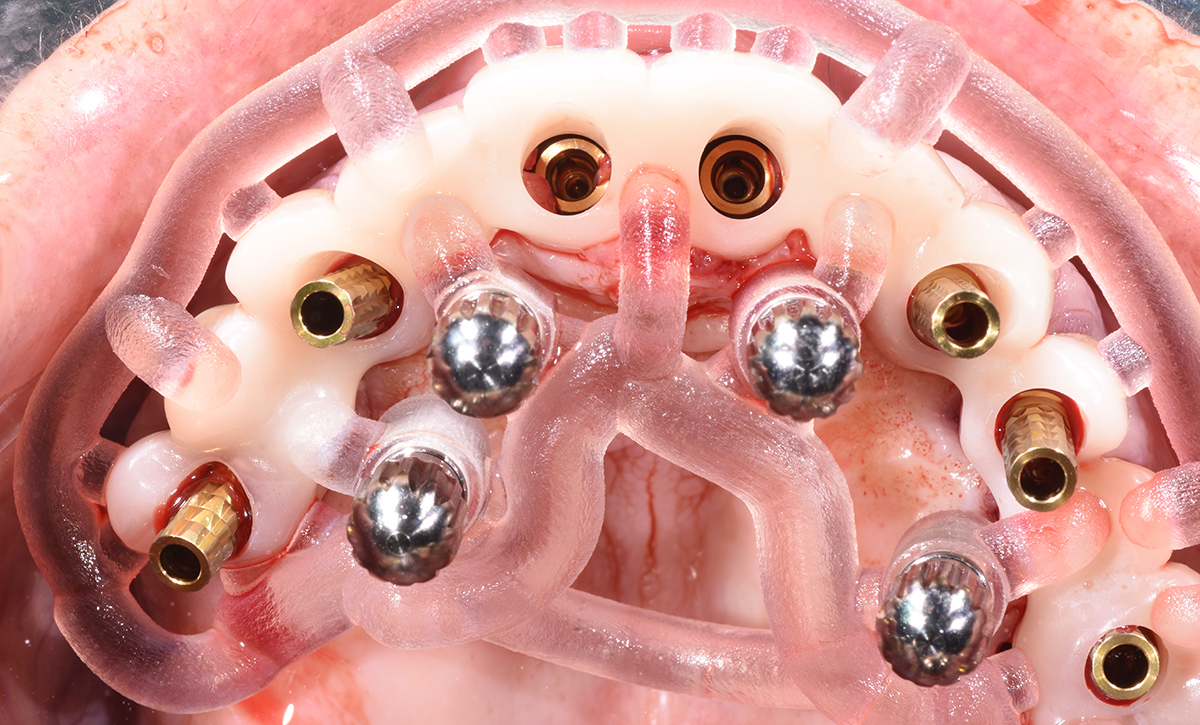
The primary stability of all implants exceeded 45 Ncm. Multi-unit and CONNECT abutments (MIS Implants, Bar Lev, Israel) were attached to the implants according the pre-prosthetic plan and were torqued to 35Ncm. Afterward, the temporary FPD was loaded into the positioning appliance and secured in the planned position using the anchor pins.