Phase IV: Laboratory Fabrication
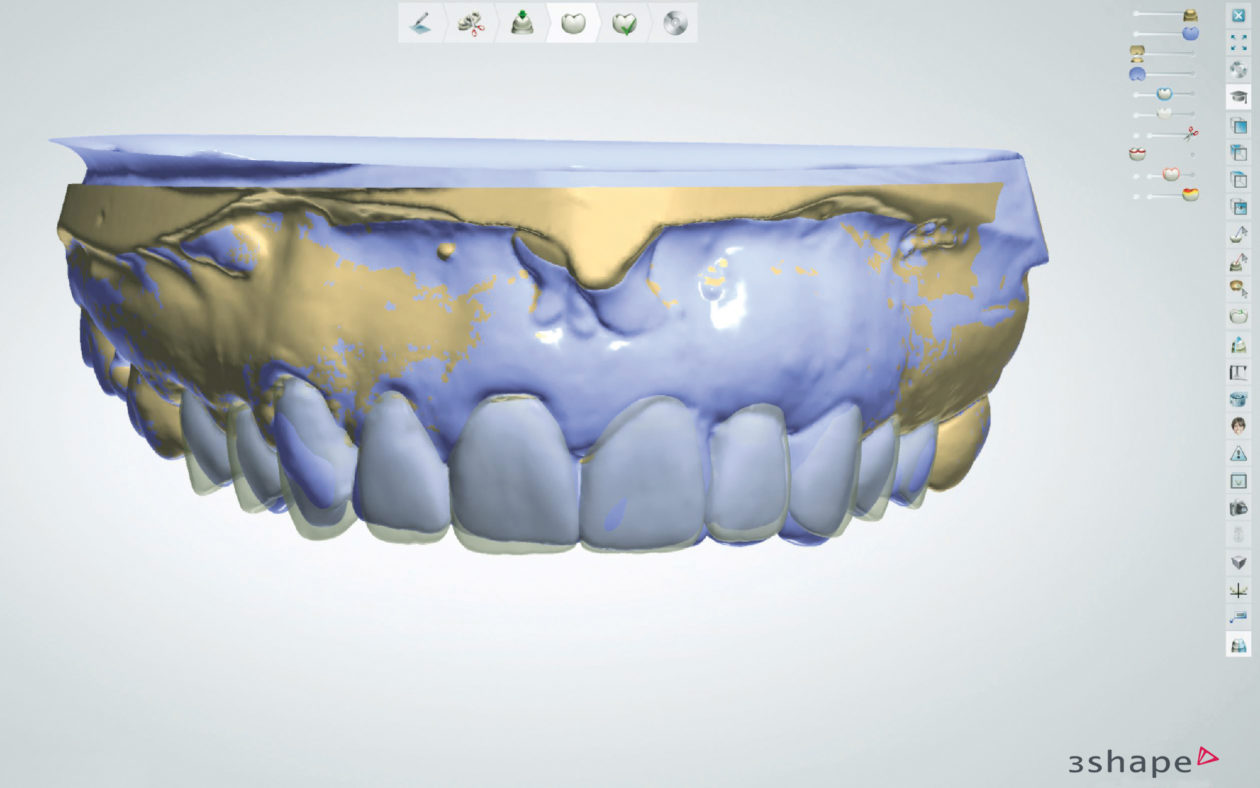
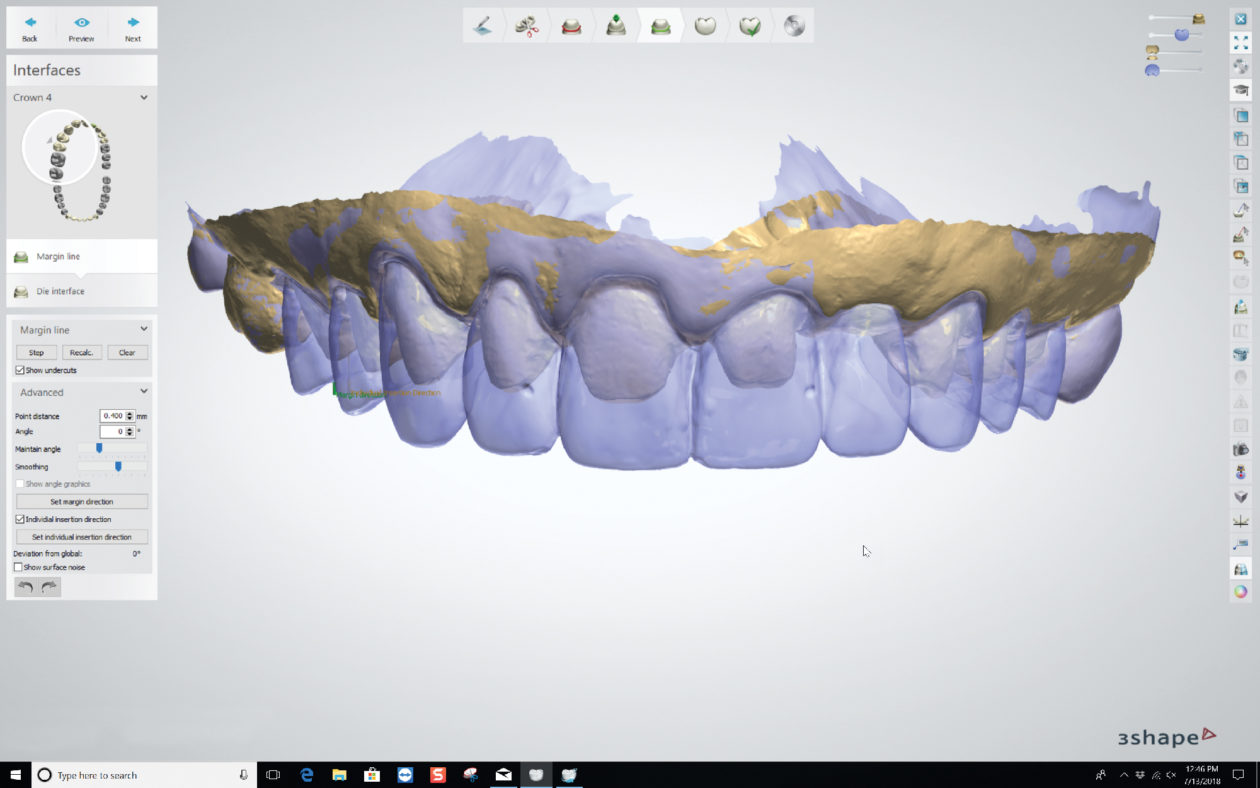
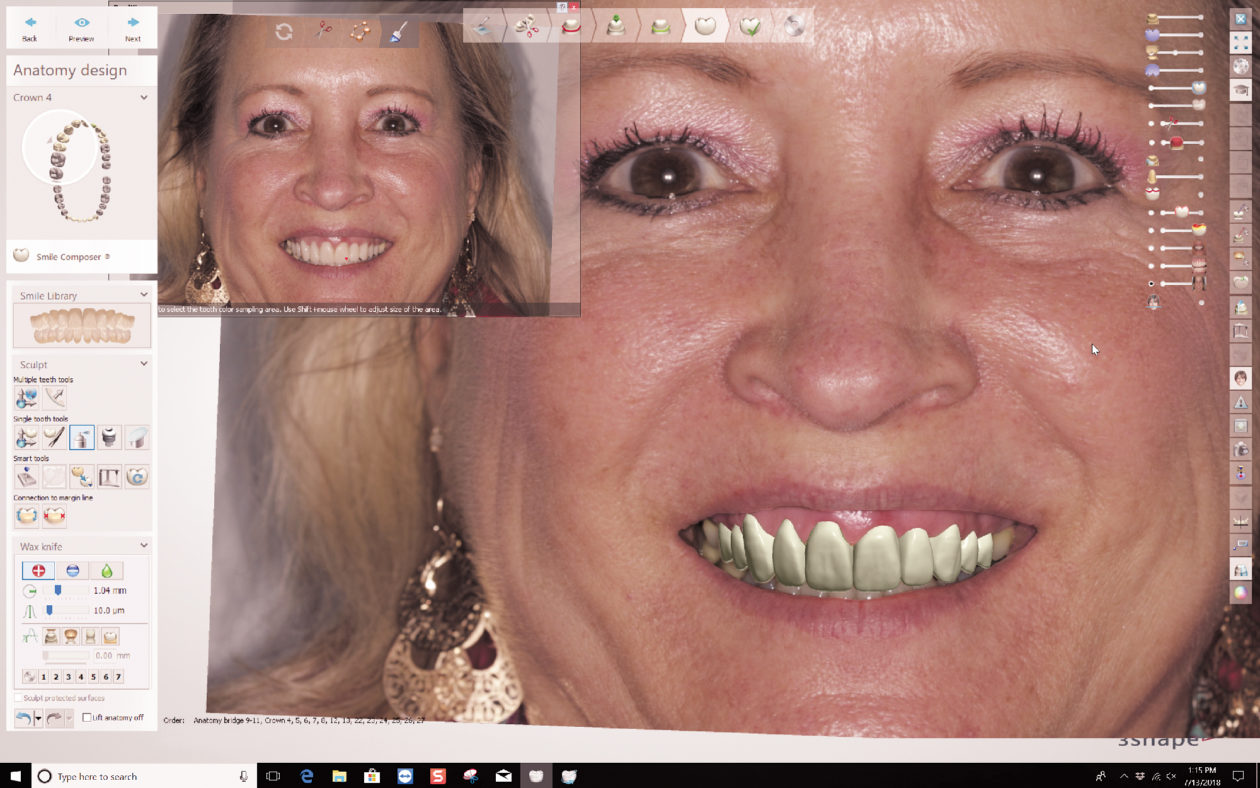
Prior to proceeding with fabrication of the definitive restorations, a full facial analysis of the provisional restorations was completed by aligning the scan of the prepared teeth, the scan of the provisionals, and a full-face smile of the patient in provisionals. The definitive restorations were digitally designed to match the form and function of the provisionals as closely as possible.
After the MT Multi zirconia bridge was milled, subtle surface morphology was added and special effects were stained into the zirconia prior to sintering. After sintering was complete, the bridge demonstrated a life-like color gradient and surface texture.
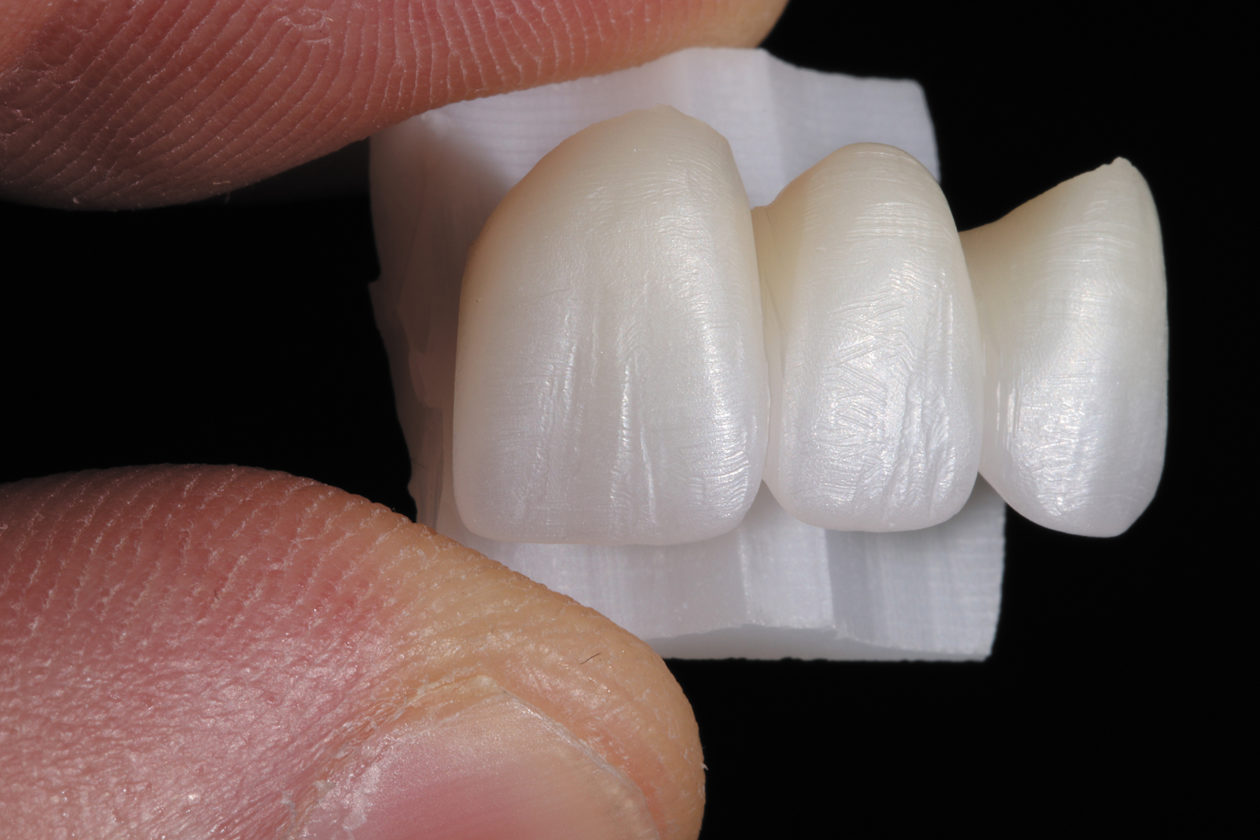
The remaining maxillary anterior zirconia restorations were milled and sintered. Staining and effects (IvoColor Staining, Ivoclar Vivadent) were applied and the color was evaluated to achieve a harmonious blend with the premolars, which were fabricated from a machinable lithium disilicate material (IPS e.max CAD). The zirconia restorations were glazed (IvoColor Glaze, Ivoclar Vivadent), ultimately enhancing the translucency and color gradient of the monolithic zirconia material.
The mandibular anterior restorations were then milled from the machinable lithium disilicate material (IPS e.max CAD) and sintered.
Phase V: Delivery Appointment
After delivery of anesthetic, the maxillary provisional restorations were removed and the definitive restorations were tried in and adjusted as needed. The patient approved the esthetics by viewing the restorations in multiple lighting situations and on photographs.
Prior to cementation, the intaglio surfaces of the zirconia restorations were cleaned with a universal cleaning paste (Ivoclean, Ivoclar Vivadent) and then rinsed and dried. Next, a self-adhesive, self-curing resin cement (SpeedCEM Plus, Ivoclar Vivadent) was loaded into the restorations. They were then seated on the preparations and the margins were tack-cured. Excess cement was easily and predictably removed.
The maxillary premolar and mandibular anterior lithium disilicate restorations were cleaned with the universal cleaning paste, rinsed, and dried. A universal primer for conditioning restoration surfaces (Monobond Plus, Ivoclar Vivadent) was applied to the intaglio surfaces of the restorations for 60 seconds, and the excess was removed. All enamel and dentin surfaces were etched with phosphoric acid for 15 seconds and thoroughly rinsed. A single-component light-cured adhesive (Adhese, Ivoclar Vivadent) was applied to the preparations, thinned, and light-cured. A neutral shade of a light- and dual-curing luting composite (Variolink Esthetic, Ivoclar Vivadent) was loaded into the restorations, and they were seated on the preparations. The restorations were tack-cured at the margins, excess cement was removed, the interproximal areas were flossed, and the restorations underwent a final cure. The occlusion was then checked and refined.
The patient returned after 3 days for further refinement of the occlusion. Records were taken for fabrication of a new bite splint, and final postoperative photographs were taken.