Phase I: Diagnostic
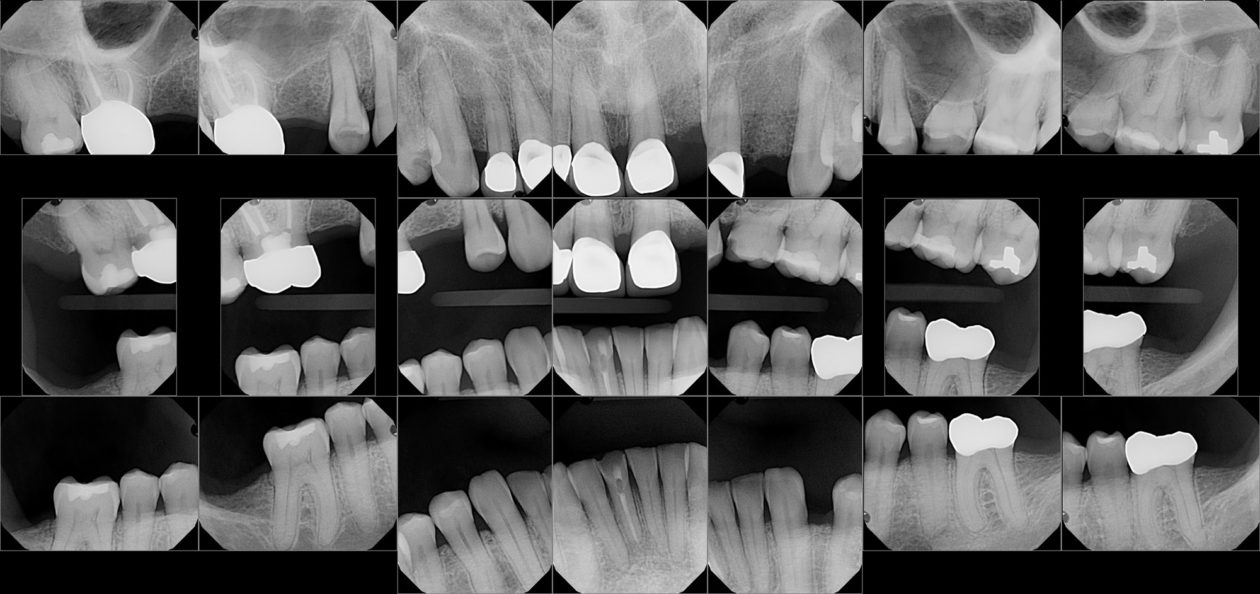
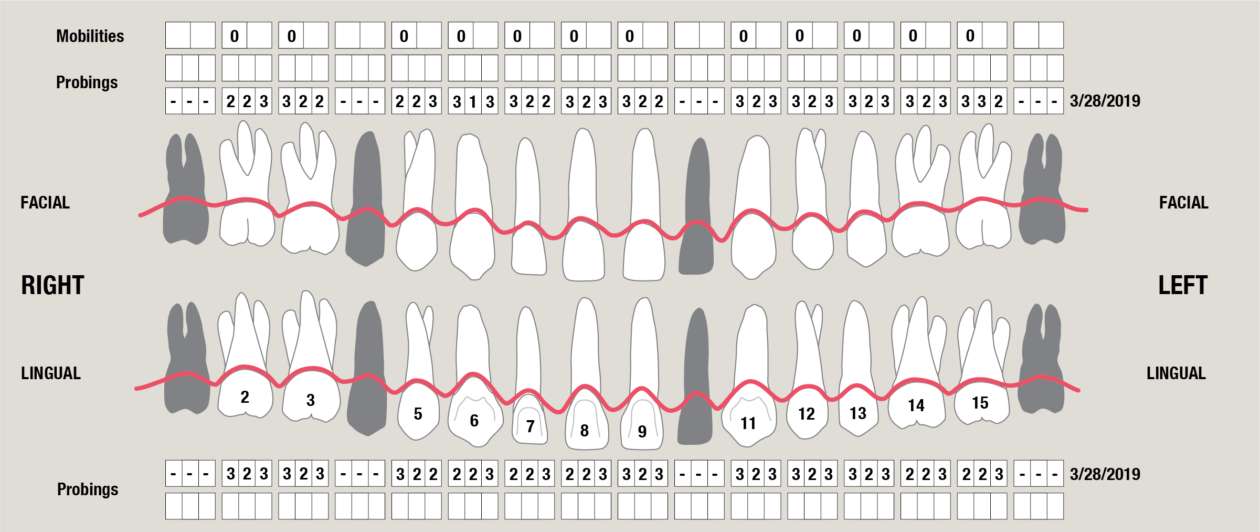
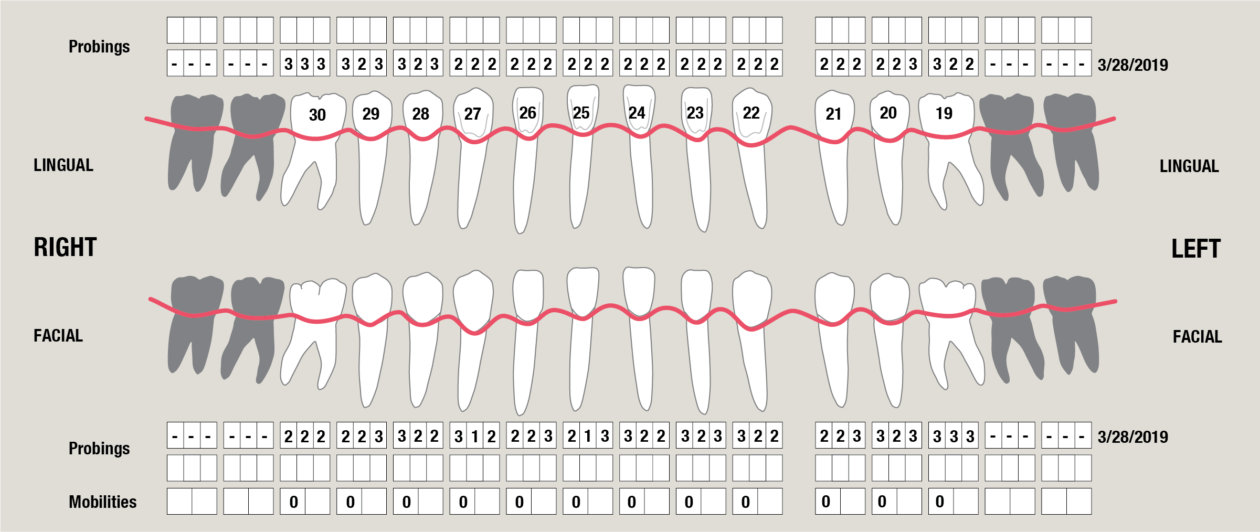
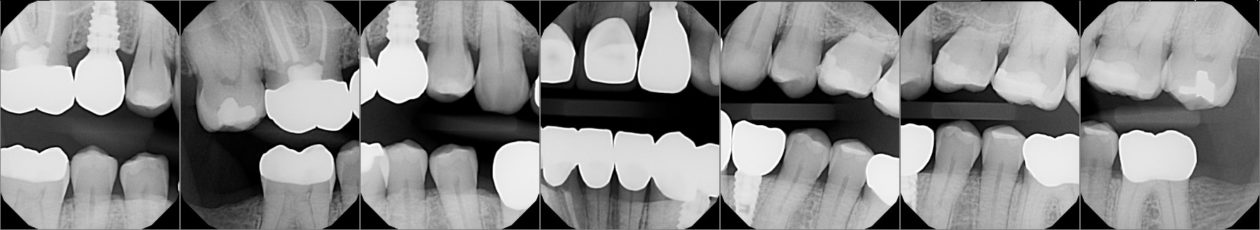
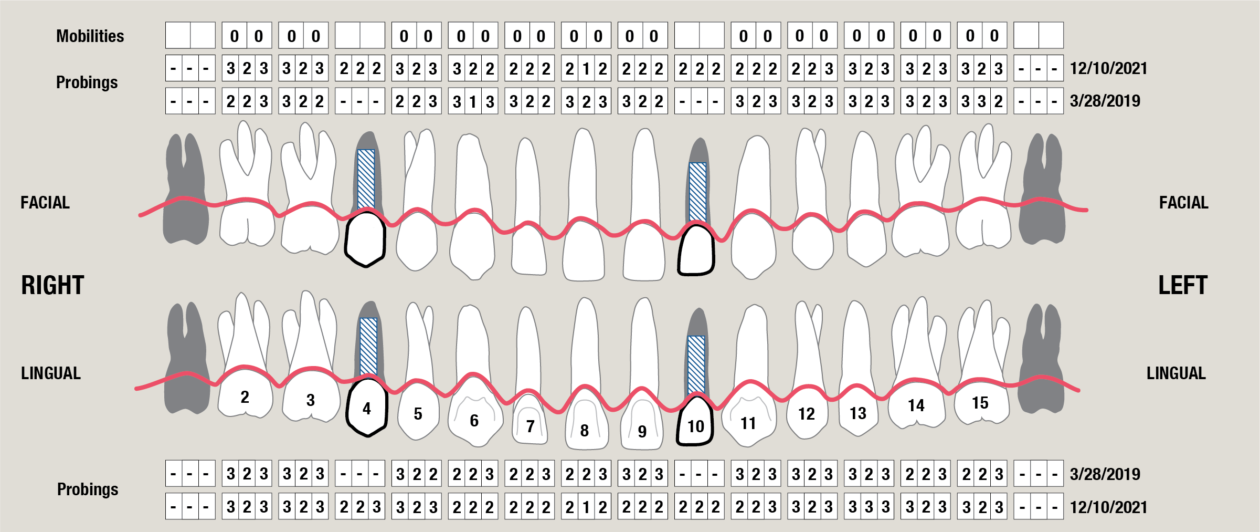
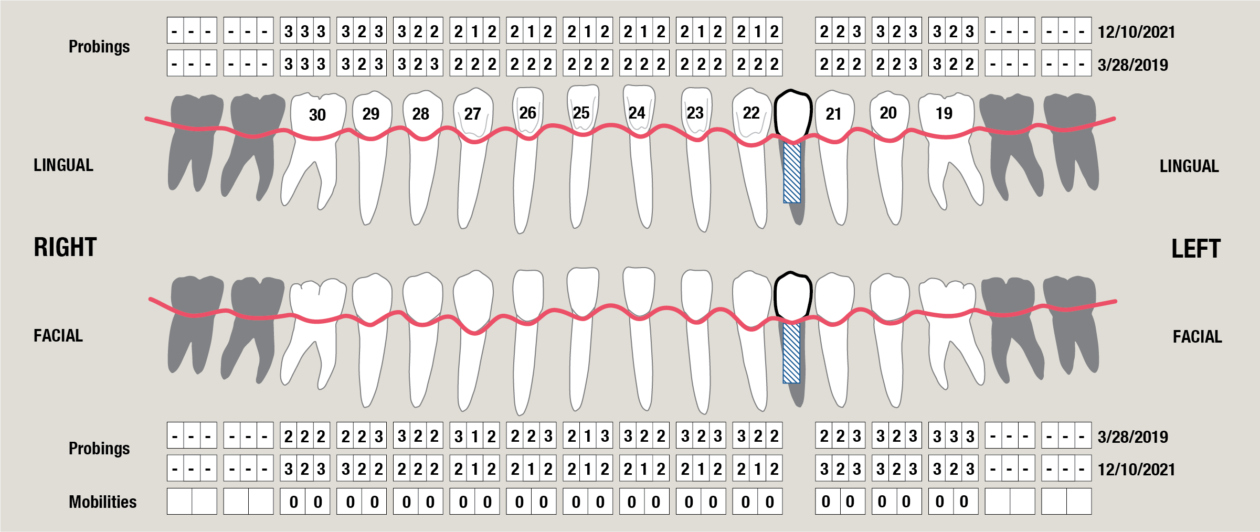
Itero scans, facebow transfer, clinical and periodontal charting, and intraoral and panoramic radiographs along with pre-op photos were obtained.
Phase II: Treatment Presentation
Multiple consultations and planning meetings were held with the restorative dentist, periodontist, orthodontist and patient to establish the final restorative plan and make sure the patient was comfortable with our approach. Having mounted models available alongside digital imaging made our treatment discussions and timeline easily understood. A thorough discussion was had regarding the compromise we were making due to the patient’s requested limitations regarding the maxillary anterior teeth. It was explained that we could achieve the best results restoratively by intruding the mandibular anterior teeth via surgical intervention. With successful intervention we would then be able to restore the appearance and function of the mandibular anterior teeth. The patient was able to see the importance of replacing the crown on tooth no. 19 and placing an onlay to tooth no. 30 to provide better posterior stops/contacts. The wax-up and pre-op photos were instrumental in helping the patient realize the importance of each planned step, and he agreed to our treatment plan.
Phase III: Hygiene Therapy
This was straightforward as the patient only had localized inflammation with localized plaque-induced gingivitis. A hygiene visit was completed with a detailed review of home care instructions and techniques in order to help the patient prepare for long-term success of his final restorations.
Phase IV: Implant Placements
A BioHorizons Tapered PLUS 4.6 x 9mm implant was placed in position no. 4 and a BioHorizons Tapered PLUS 3.8 x 12mm implant was placed in position no. 10.
Phase V: Surgically Facilitated Orthodontics
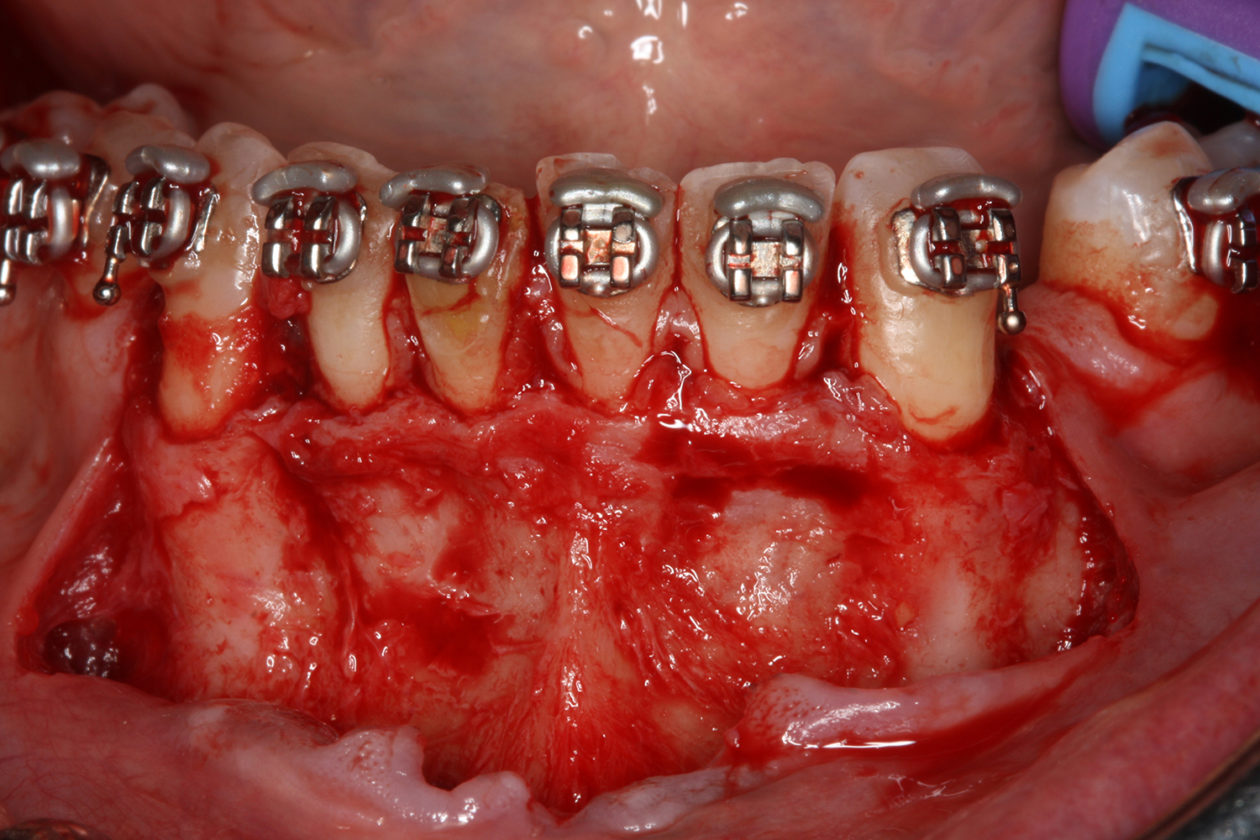
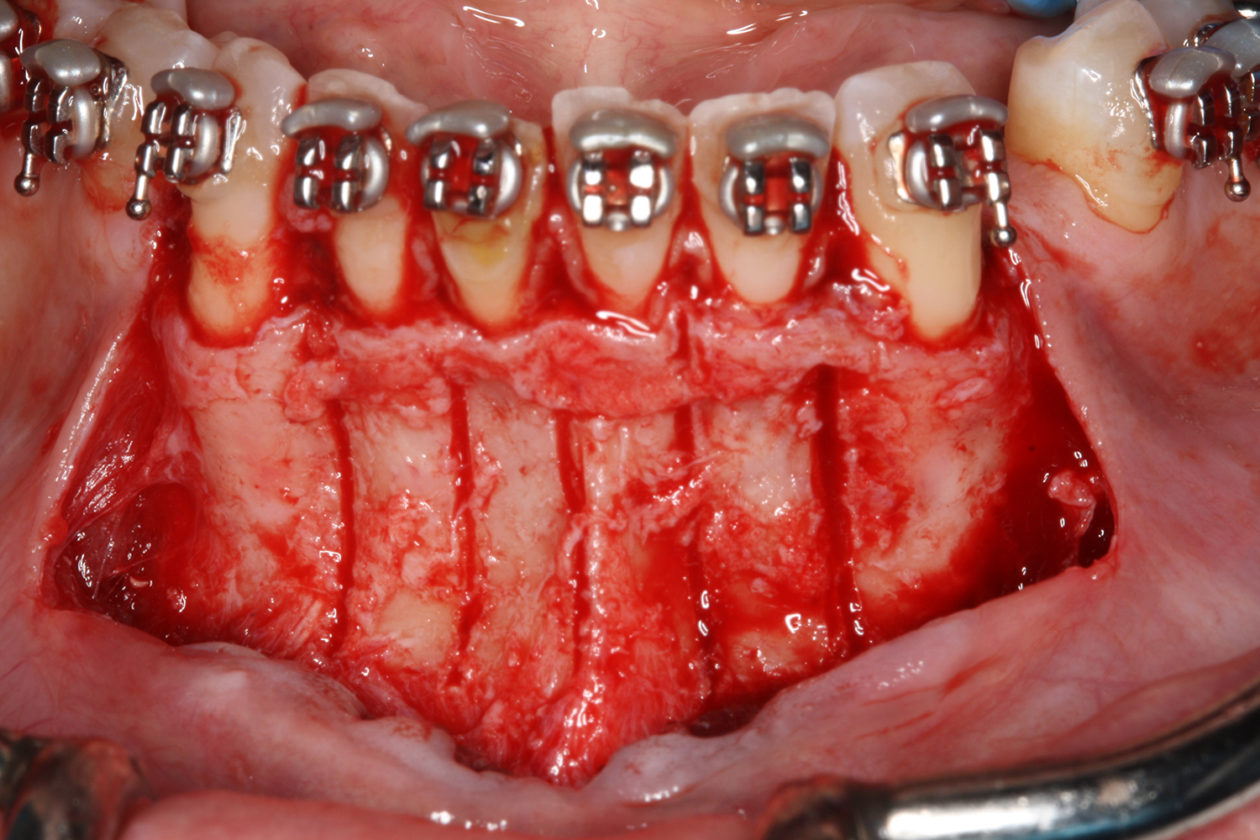
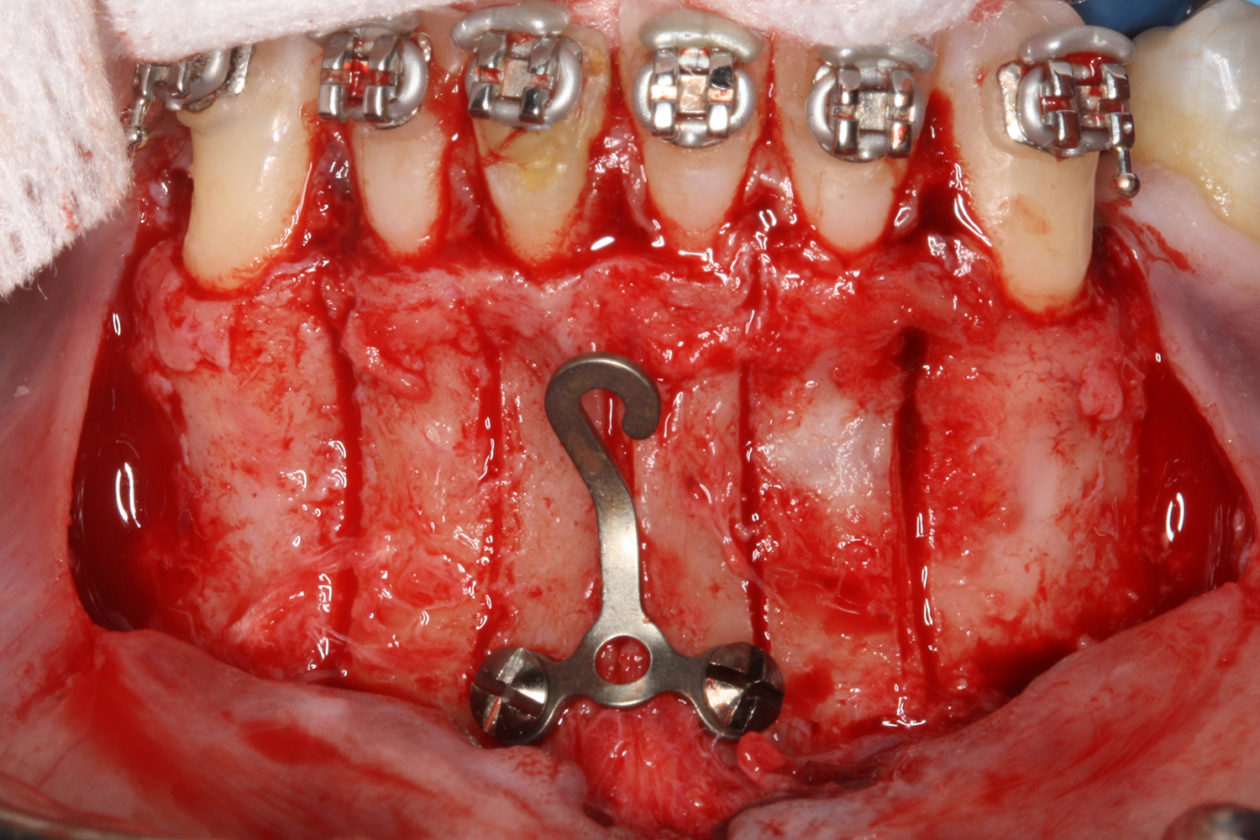
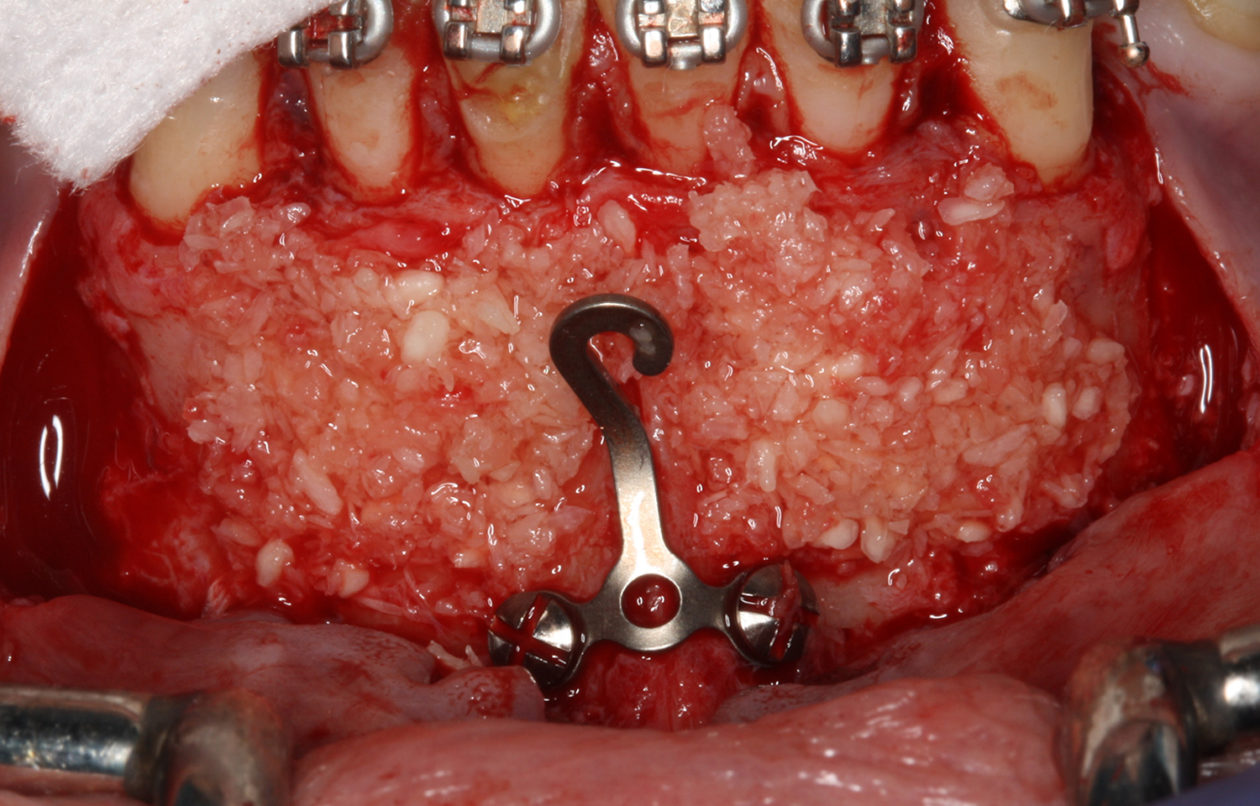
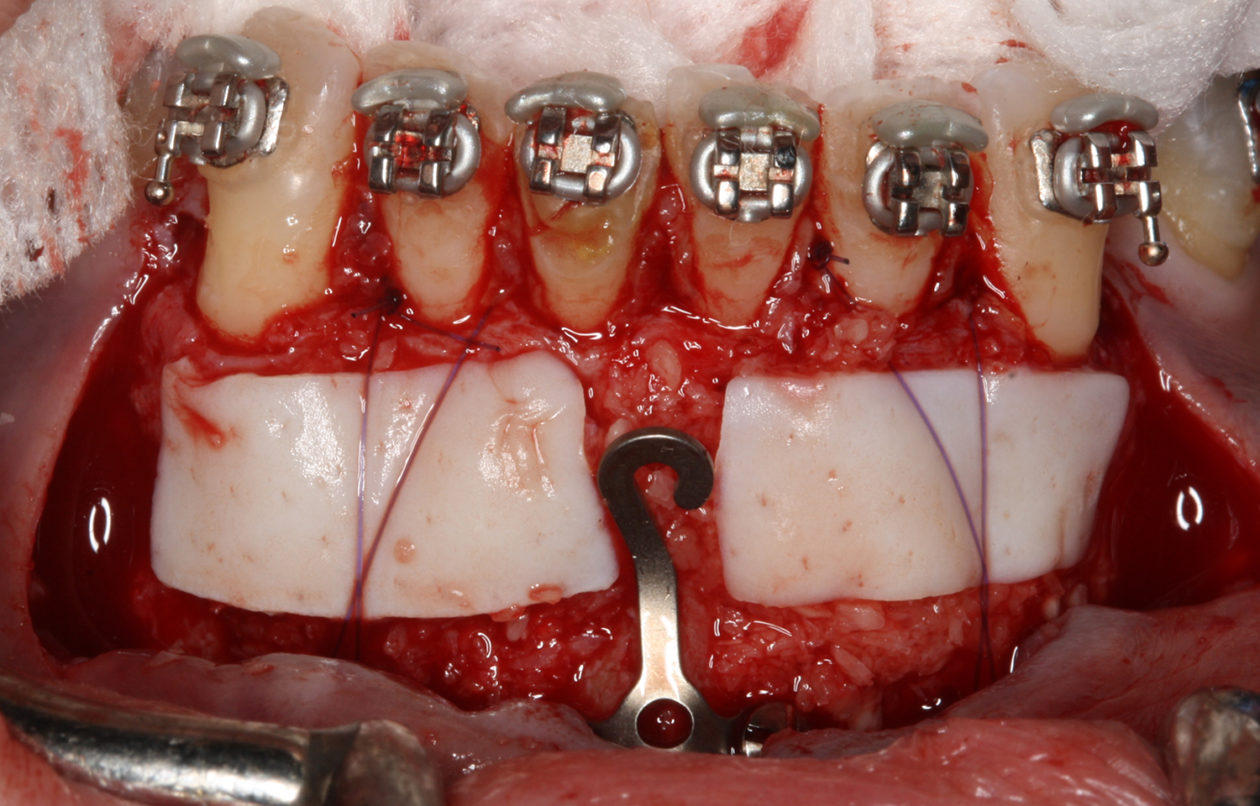
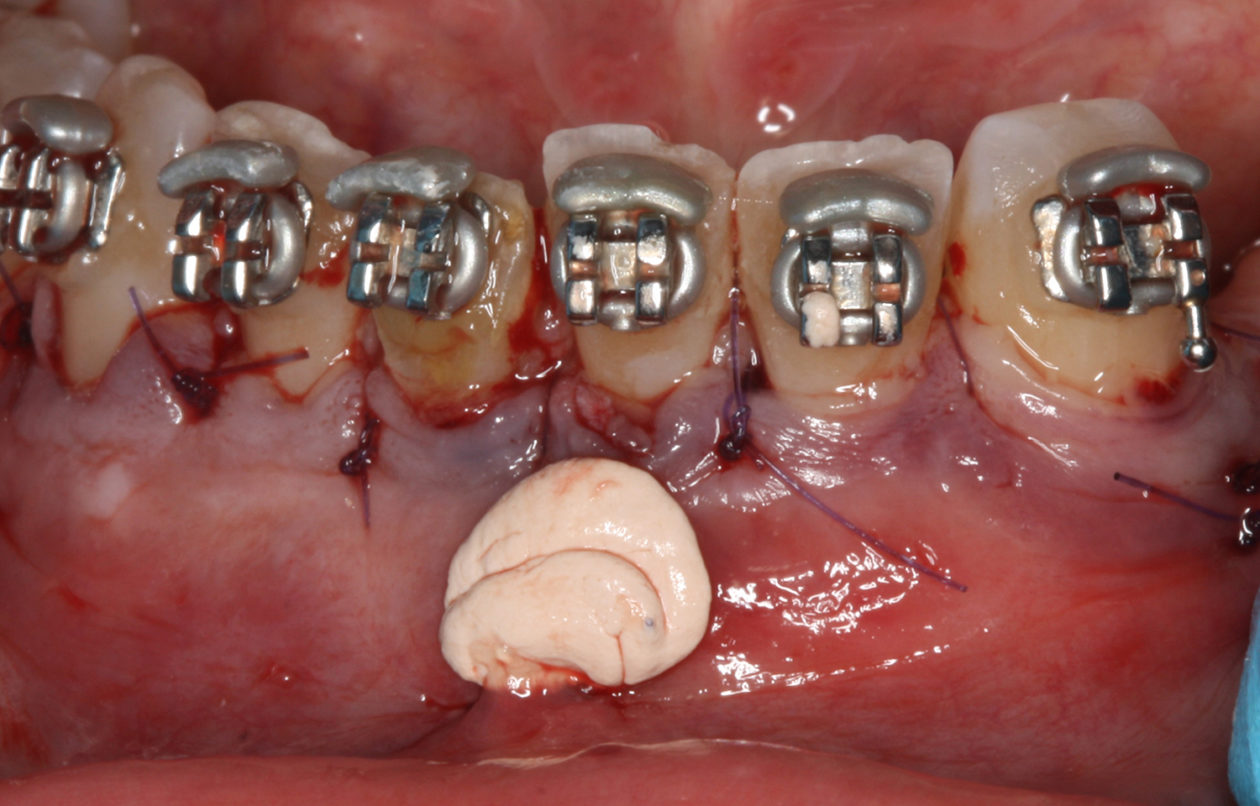
The orthodontic goal was to intrude the mandibular anterior teeth to provide more prosthetic space for the future restorations on teeth nos. 22, 23, 24, 25, 26, and 27. After brackets were placed on the mandibular arch, surgical access was created with vertical releasing incisions distal to teeth nos. 22 and 27, and intrasulcular incisions from tooth no. 22 to tooth no. 27. Selective corticotomies took place utilizing piezosurgery. The surgical mini-plate was manually shaped to accommodate installation on the symphysis, and then stabilized with screws. Onlay grafting was followed with cortical cancellous mineralized particulate allograft infused with A-PRF (advanced platelet-rich fibrin). In order to further enhance soft tissue phenotype, an allogenic dermal matrix was placed and stabilized with periosteal sling resorbable sutures. Advancement of the flap and closure was completed after the mucosa was perforated to accommodate access to the mini-plate’s hook.
At the completion of orthodontics, re-entry for retrieval of the surgical mini-plate took place utilizing a mucosal incision. This prevented disturbance of the gingival margins of the mandibular anterior teeth.
















Social History
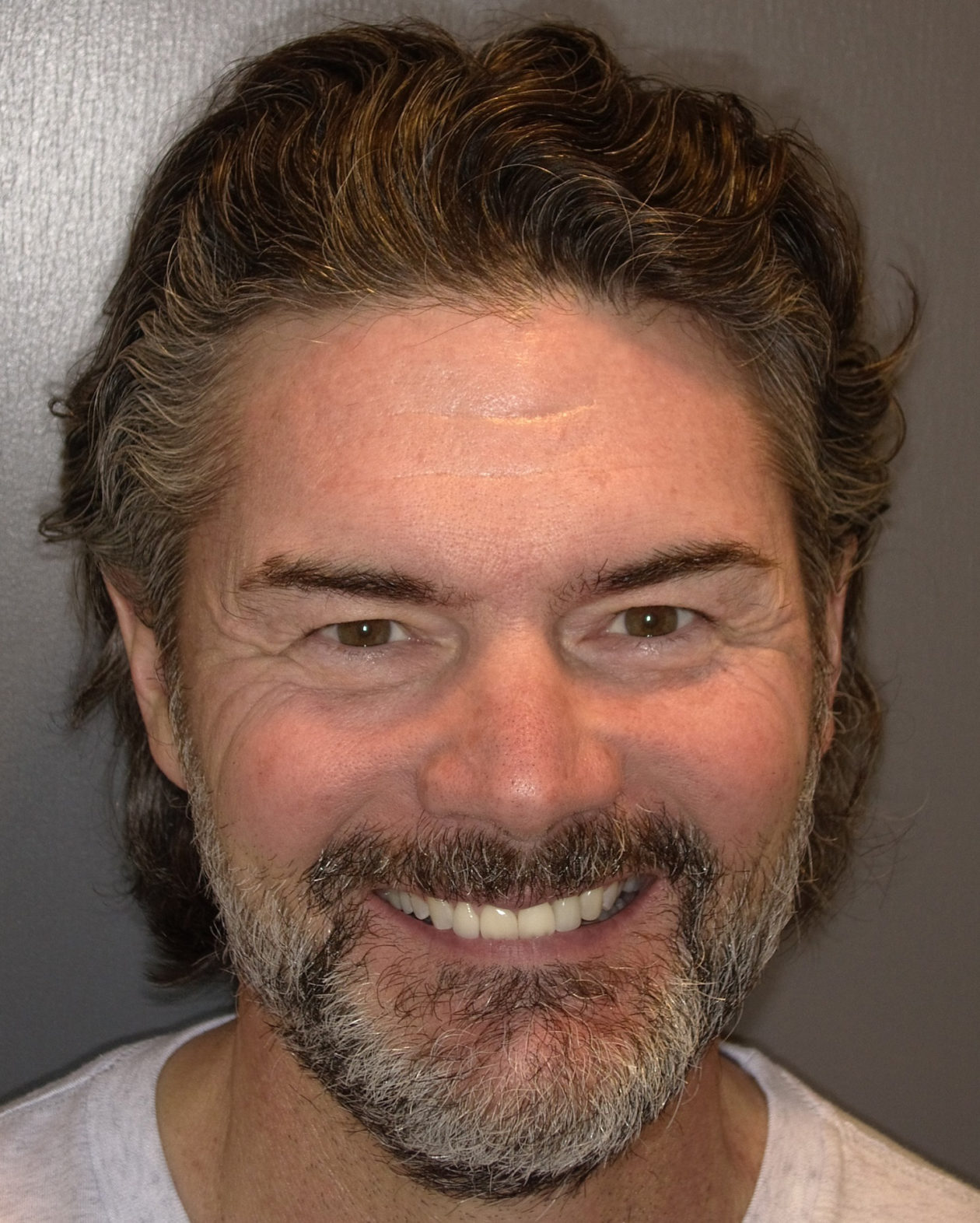
The patient is a high-profile person who entertains and lectures to clients. He had a high demand for an esthetic solution where he would not be in temporaries that would break or cause problems while he traveled. He also did not want to make any changes/improvements to his existing anterior crowns as he liked the color and appearance.