Dr Shouresh Charkhandeh, Dr John Remmers & Paul Cataford
Sleep-related breathing disorders (SRBD) and obstructive sleep apnea (OSA) affect millions of people in America and are associated and prevalent with a number of other health-related issues, including stroke, obesity, diabetes, heart disease, drug-resistant hypertension, coronary artery disease, cardiac arrhythmias, congestive heart failure, depression, and anxiety. In addition, poor sleep may lead to moodiness, impaired concentration, a higher risk of automobile or industrial accidents, and reduced work efficiency.
In addition to the health effects described, there are a number of oral health issues related to SRBD. In fact, over the past decade, studies have demonstrated the impact of untreated SRBD on dentistry and the prognosis of many dental treatments.
Sleep and Dentistry
Treating sleep is an integral part of inter-disciplinary dentistry.
Sleep and Bruxism [1,2]
One of the most well-studied topics is the connection between SRBD and bruxism. It seems some people clench when they struggle to breathe when sleeping. In the past, dentists have treated the symptom and put bumpers in place (night guards) and missed the opportunity to treat the root cause issue, which may be SRBD. Worse, in some cases, bruxing guards may make the effects of the SRBD more severe. A simple sleep screen and test may tell you what the right treatment strategy should be.
With so many different treatment strategies impacted by the presence of bruxism, many dentists would be prudent to consider the possible impact of untreated or undiagnosed SRBD during the data gathering phase of treatment planning. This is essential because studies show a significant reduction of sleep bruxism in patients with OSA when proper mandibular repositioning devices are used to manage the OSA.
Sleep and Periodontal Therapy[3,4,5]
Studies show that proper periodontal care reduces health risks. New studies show there is also a significant association between untreated SRBD and periodontal disease. The exact mechanism by which one affects the other is still being studied; however, the high prevalence of periodontal disease in SRBD patients has been attributed to:
- High prevalence of mouth breathing in SRBD patients,
- Compromised immune response in SRBD patients, which adversely impacts healing required for periodontal disease management,
- High level of systemic inflammation in SRBD patients, which also impacts the patient’s periodontal status.
The inflammatory nature of periodontal diseases becomes more important when studies show sleep apnea treatment improves the levels of inflammatory markers in SRBD patients. Considering the prevalence of periodontal disease and how different treatment modalities and protocols have been tested or recommended, as dentists, we must consider the impact of SRBD on our periodontal treatment plans.

Sleep and Ortho[6,7]
Dentofacial and craniofacial development also relies on proper breathing and sleep. Children with breathing, airway disorders, sleep issues, and improper craniofacial growth have an increased risk for developing retrognathia. In addition, these craniofacial abnormalities may also increase the risk factor for children to develop OSA. Of course, the impact of OSA in children goes well beyond the craniofacial development and can adversely impact their learning, emotions and behavior. The high prevalence of ADHD in pediatric OSA patients is another reason why early recognition and treatment of SRBD is so important. When dentists consider the role airway anatomy plays in OSA and the possible impact of orthodontic and orthopedic treatments, it becomes clear that OSA screening must be part of every orthodontic data gathering and treatment planning phase.
Sleep and TMD, Surgery and Implantology[8,9,10,11]
Recent studies identify patients with OSA have an increased risk of developing TMD, possibly due to a higher level of serum inflammatory markers (such as IL-6, IL-8, C-reactive protein, etc.). Typically, OSA patients heal slowly and have a higher pain perception (i.e. hyperalgesia) due to lack of REM sleep. These factors may significantly impact the prognosis of TMD and pain management. The factors, combined with sleep bruxism, may explain why OSA patients have a higher incidence of restorative failure in implant dentistry.
Sleep and airway assessment must be part of comprehensive treatment planning and form the basis of interdisciplinary dentistry.
Untreated SRBD can have significant adverse impacts on the prognosis for many dental procedures, and if ignored, SRBD can compromise the longevity of dental care. The question is not whether sleep and airway management should be part of our comprehensive assessment, but how and where it fits.
Dentists agree that screening is part of dentistry, but we must provide answers on how screening impacts the dentist’s overall treatment planning and treatment sequence. Questions include:
- What takes priority in the treatment planning phase?
- At which phase of treatment does SRBD need to be addressed?
- What if the patient does not want to proceed with any therapy?
- How can we minimize/manage the impact of OSA on our dentistry?
- Is every patient who responds to mandibular protrusion a good candidate for OAT? Even if they have enough teeth?
- What is the role of adjunctive therapies and some newer and promising treatment modalities?
- Is sleep a specialty-driven discipline or is it part of everyday dentistry?
- How should a general practitioner treatment plan OSA-positive patients?
- Can OSA treatment be delayed until a different dental treatment phase is completed?
The answers to these questions are essential if we, as dentists, want to be more effective. It remains clear that our progression and pursuit of comprehensive treatment planning for airway and sleep must be considered first to achieve predictable outcomes, avoid surprises, and improve clinical prognosis.
As airway and breathing impacts everything, analysis should come before function, biology, and aesthetics in treatment planning.
Okay, SRBD is bad stuff, but why should a dentist be concerned and what role does the dentist play in dealing with this medical illness?
The answer is simple, a dentist can now treat it.
In the past, dentists could always take impressions and make appliances, but treating a medical disease was always out of scope. In the past, in order to determine if the treatment was effective, a patient would have to be sent back to the physician to complete a test, with the appliance, to see if it worked. Unfortunately, it only worked in about 60 percent of the cases, and with a $3,000-4,000 treatment fee, patients and dentists didn’t want to take the risk. Further, we’ve learned adjusting the appliance in an anterior-posterior plane provided different outcomes and results. Guesswork and failure—things Seattle Study Club dentists won’t tolerate.
The past is the past.
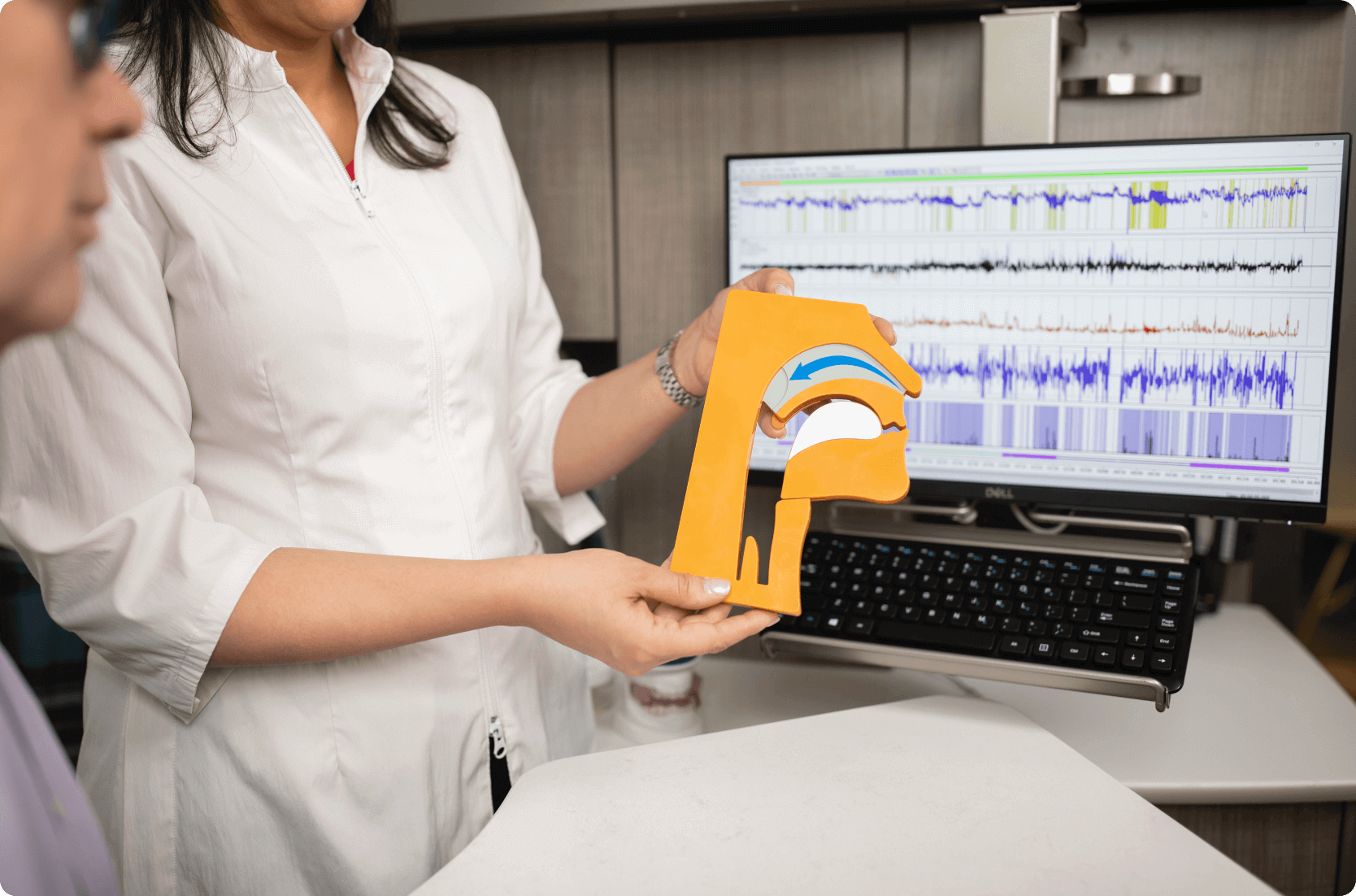
A Seattle Study Club partner, Zephyr Sleep Technologies has cleared the way with the recent release and FDA clearance of the MATRx plus™ Treatment Planning System. Zephyr has more than 350 users of the medical device and workflow already and is on the second generation of the system.
Now, dentists can finish a treatment plan after completing a two-night MATRx plus test in advance of treatment and know if the sleep appliance will treat the illness and how to custom configure the appliance for effective treatment. In fact, the MATRx plus can also complete a home sleep test, if the patient needs to be diagnosed.
Want to learn more? Visit zephyrsleep.com.
References
Bruxism:
1. Oksenberg A, Aarons E. Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Sleep Med. Nov. 2002; 3(6):513-515.
2. Mayer P, Morisson F, Rompré PH, Lavigne GJ. Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients. Int J Prosthodont. Jul.-Aug. 2004;17(4):447-453.
Sleep and Periodontal Therapy:
3. Seo WH, Cho ER, Thomas RJ, An SY, Ryu JJ, Kim H, Shin C. The association between periodontitis and obstructive sleep apnea: a preliminary study. J Periodontal Res. Aug. 2013;48(4):500-506. doi: 10.1111/jre.12032. Epub Nov 30, 2012.
4. Gunaratnam K, Taylor B, Curtis B, Cistulli P. Obstructive sleep apnoea and periodontitis: a novel association? Sleep Breath. Aug. 2009;13(3):233-239. doi: 10.1007/s11325-008-0244-0. Epub Feb. 6, 2009.
5. Baessler A, Nadeem R, Harvey M, Madbouly E, Younus A, Sajid H, Naseem J, Asif A, Bawaadam H. Treatment for sleep apnea by continuous positive airway pressure improves levels of inflammatory markers – a meta-analysis. Journal of Inflammation 2013;10:13.
Sleep and Ortho:
6. Harari D, Redlich M, Miri S, Hamud T, Gross M. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope. Oct. 2010;120(10):2089-2093. doi: 10.1002/lary.20991.
7. Villa MP, Rizzoli A, Miano S, Malagola C. Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. Sleep Breath. May 2011;15(2):179-84. doi: 1007/s11325-011-0505-1. Epub Mar. 25, 2011.
Sleep and TMD, Surgery and Implantology:
8. Roehrs T, Hyde M, Blaisdell M, Greenwald M, Roth T. Sleep loss and REM sleep loss are hyperalgesic. SLEEP 2006;29(2).
9. Sanders AE, Essick GK, Fillingim R, Knott C, Ohrbach R, Greenspan JD, Diatchenko L, Maixner W, Dubner R, Bair E, Miller VE, Slade GD. Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res. Jul. 2013;92(7 Suppl):70S-7S. doi: 10.1177/0022034513488140. Epub May 20, 2013.
10. Incidence of Prosthetic Complications associated with Implant-borne Prosthesis in a Sleep Disorder Center. Venkatesh B Suneel 1, Santhosh Kotian 2, Ravikanth H Jujare 2, Adarsh K Shetty 3, Sneh Nidhi 4, Shehkar Grover 5
11. Frequency of Prosthetic Complications Related to Implant-Borne Prosthesis in a Sleep Disorder Unit. Anitua E, Saracho J, Almeida GZ, Duran-Cantolla J, Alkhraisat MH.J Oral Implantol. 2017 Feb;43(1):19-23. doi: 10.1563/aaid-joi-D-16-00100. Epub 2016 Oct 4.PMID: 27700231



