Greg Asatriana
a Private Practice, 17220 Newhope St #227, Fountain Valley, CA 92708
Address all Correspondence to:
Greg Asatrian, DDS, MS
gasatrian@gmail.com
Abstract
Introduction: One of the biggest obstacles faced by dental professionals when managing orthodontics patients is the maintenance of adequate oral hygiene.
Methods: Seven teenage patients with fixed orthodontic appliances and poor oral hygiene were evaluated before and after four weeks of incorporating an oscillating-rotating (O-R) toothbrush with a novel brush head for special focus areas. Baseline and follow-up patient surveys, intraoral photos, plaque and gingival indices, and orthodontic plaque indices were collected. Oral hygiene instructions with the O-R toothbrush and Targeted Clean brush head were provided and all other oral hygiene routine protocols and products were to remain unchanged.
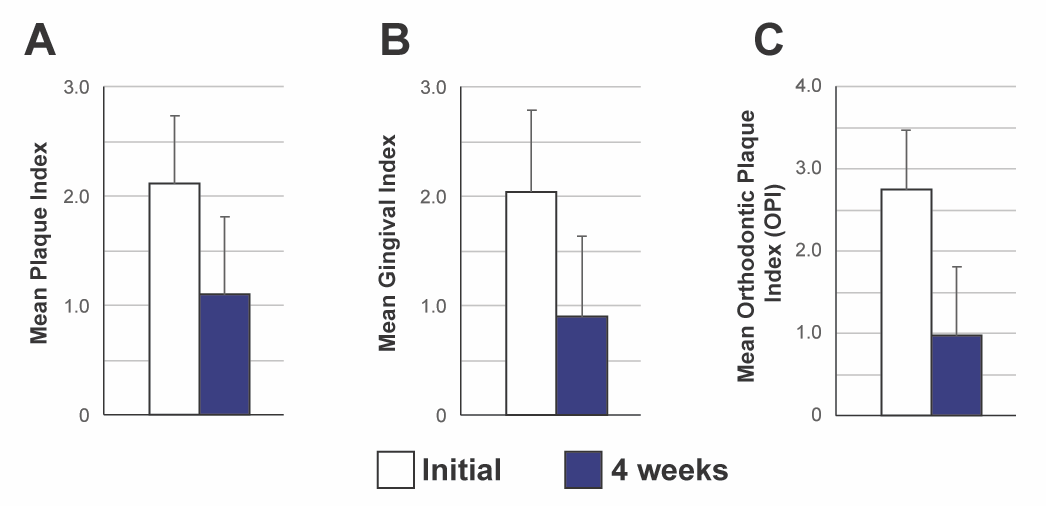
Result: Mean initial plaque and gingival indices were 2.04 and 2.12, respectively, revealing moderate accumulation of plaque with redness, edema and glazing of the gingival margin. At follow-up, a clinically meaningful improvement was observed with a mean decrease in the plaque index by 1.14 (SD 0.78) and gingival index by 1.01 (SD 0.70). Six of seven patients reported that they were more motivated to brush and all reported that they brushed longer and had cleaner feeling teeth.
Conclusion: Clinically meaningful improvements with the use of a novel electric O-R toothbrush head were observed in orthodontic patients with poor oral hygiene.
Introduction
Over the past several years we have witnessed a consistent increase in the public’s interest in undergoing orthodontic treatment.1 It is fantastic to see more individuals improving their occlusion, function, and confidence with improved aesthetics. It is important, however, that patients are aware of the risks, potential consequences of treatment as well as their own responsibility to help ensure their treatment success. One of the biggest obstacles faced by dental professionals when managing orthodontic patients is the maintenance of adequate oral hygiene and the mitigation of the sequelae of inadequate plaque control.2 It is without a doubt that maintenance of oral hygiene is further compounded by the complexity of cleaning around fixed orthodontic appliances. As such, during orthodontic treatment, caries, decalcification, and gingivitis occur in up to 96% of all patients, depending on the clinical measurement being assessed.3 Moreover, childhood gingivitis is diagnosed in 80% of 11- to 13- year olds, a patient demographic which coincides with the most frequent age to undergo orthodontic treatment.4 These declines in oral hygiene have been shown to increase orthodontic treatment length due to increased binding of tooth movement (calculus between teeth and inside of orthodontic bracket tubes), broken brackets, and restorative/periodontal needs. In fact, studies have shown that for each appointment where a patient is reported to have poor oral hygiene, his/her treatment length is likely to increase by 0.67 months.5, 6 Unfortunately, this increase in treatment length can have a detrimental impact on the oral health of patients who are already struggling to maintain proper hygiene, as well as disrupt the clinical flow of the practice due to an increasing number of help/emergency visits. Dental professionals combat this increased tendency for a decline in oral hygiene by consistent oral hygiene instruction, education, and more frequent prophylactic hygiene visits, however in conjunction to these efforts, the patient must be equipped with a proper oral hygiene armamentarium at home.
The primary preventative tool for mitigating plaque accumulation is mechanical disruption of biofilm and several systematic reviews and meta-analyses have shown that electric toothbrushes are significantly more efficacious when compared to manual toothbrushes at doing just that.7, 8 Within the realm of manual and power toothbrushes, recent systematic reviews and meta-analyses7, 9, 10 have revealed that oscillating-rotating (O-R) technology provides superior gingival health benefits when compared to other technologies (such as sonic), in particular with adolescent and orthodontic patients.11-13
Since the advent of O-R technology in 1991 there have been improvements to the system including increased oscillation-rotations, optimized brush head design, as well as added features such as smart pressure indicators, timers and Bluetooth-linked applications. These features support patient modifications in behavior to improve their oral hygiene routine by brushing for the appropriate amount of length and ensuring all surfaces of the oral cavity are being brushed. The most recent addition to the O-R power toothbrush family is the Oral-B iO with a linear magnetic drive system, bi-modal smart pressure indicator and redesigned brush heads. In an 8-week period, the odds of transitioning from “not healthy” to “healthy” gingival status when using this brush were 14.5 times higher when compared to participants who used a manual toothbrush, and 4.75 times higher when compared to participants using a sonic brush .14, 15
In this study, we evaluated the impact an O-R toothbrush (Oral-B iO), coupled with the novel brush head (Oral-B Targeted Clean; TC), has on orthodontic patients with poor oral hygiene, compliance and existing gingivitis. The TC brush head (Fig. 1) was designed with dental professionals for effective plaque control around braces, implants, and other areas that require special focus. Its design facilitates localized plaque removal and, as the name implies, assists cleaning targeted loci.

Materials & Methods
To evaluate the effectiveness of the O-R power brush in conjunction with the TC brush head, seven patients were selected and evaluated at the beginning of the study and after a four-week period. Subjects were screened prior to involvement in this case series evaluation and their medical and dental history were reviewed. To participate, subjects were required to be at least 12 years of age, healthy, have fixed orthodontic appliances in both arches, with poor oral hygiene, and not have received a professional cleaning in the past 3 months.
At the initial visit, patients were surveyed on their self-perceived oral health. Patients were asked to score their oral hygiene on a scale of 0-5, with zero representing very bad and five representing very good. Moreover, patients were asked to rate how clean their teeth felt after cleaning on a scale of 0-5, again with zero representing very dirty and five representing very clean. Lastly, patients self-reported how many times per day they brush their teeth, and for how long on average.
Subsequently, intraoral photos were captured and measurements were captured on the Ramfjord teeth. The assessed teeth consist of the maxillary right first molar (#3), maxillary left central incisor (#9), maxillary left first bicuspid (#12), mandibular left first molar (#19), mandibular right central incisor (#24) and mandibular right first bicuspid (#28). First, plaque index measurements were performed on the aforementioned teeth at four sites (buccal, lingual, mesial and distal) and were scored as follows: 0, no plaque; 1, thin plaque at the gingival margin; 2, moderate accumulation with plaque in the sulcus; 3, large amount of plaque in the sulcus or pocket along the free gingival margin. On the same teeth, and at the same sites, Löe-Silness Gingival Index measurements were recorded as follows: 0, normal gingival with natural coral pink gingival with no signs of inflammation; 1, mild inflammation with slight changes in color and slight edema (no bleeding on probing); 2, moderate inflammation with redness, edema and glazing (bleeding on probing), 3; severe inflammation with marked redness, edema, ulceration and tendency to bleed spontaneously. Lastly, orthodontic plaque index (OPI) was measured which quantifies the amount of plaque around the orthodontic appliances. OPI is calculated per sextant and scored as follows: 0, brackets are plaque-free; 1, isolated plaque islands on one tooth surface at the bracket base; 2, plaque on two tooth surfaces at the bracket base; 3, plaque on three tooth surfaces at the bracket base; 4, plaque on all the tooth surfaces at the bracket base and/oral gingival inflammation.
Patients were then provided oral hygiene instruction on how to properly use an O-R toothbrush with the novel TC brush head. Subjects were instructed to brush twice daily for two minutes using the Ultimate Clean brush head and then follow up for one minute, twice daily, using the novel TC brush head. Subjects were instructed to use the TC brush head on Interproximal surfaces and inter-bracket surfaces. All other oral hygiene products and regimens were instructed to remain unchanged, including their usual toothpaste, water flosser, interdental cleaner, etc. After four weeks of use, patients were recalled and the same oral hygiene indices were evaluated, intraoral photos captured, and a post-study survey obtained.
Results
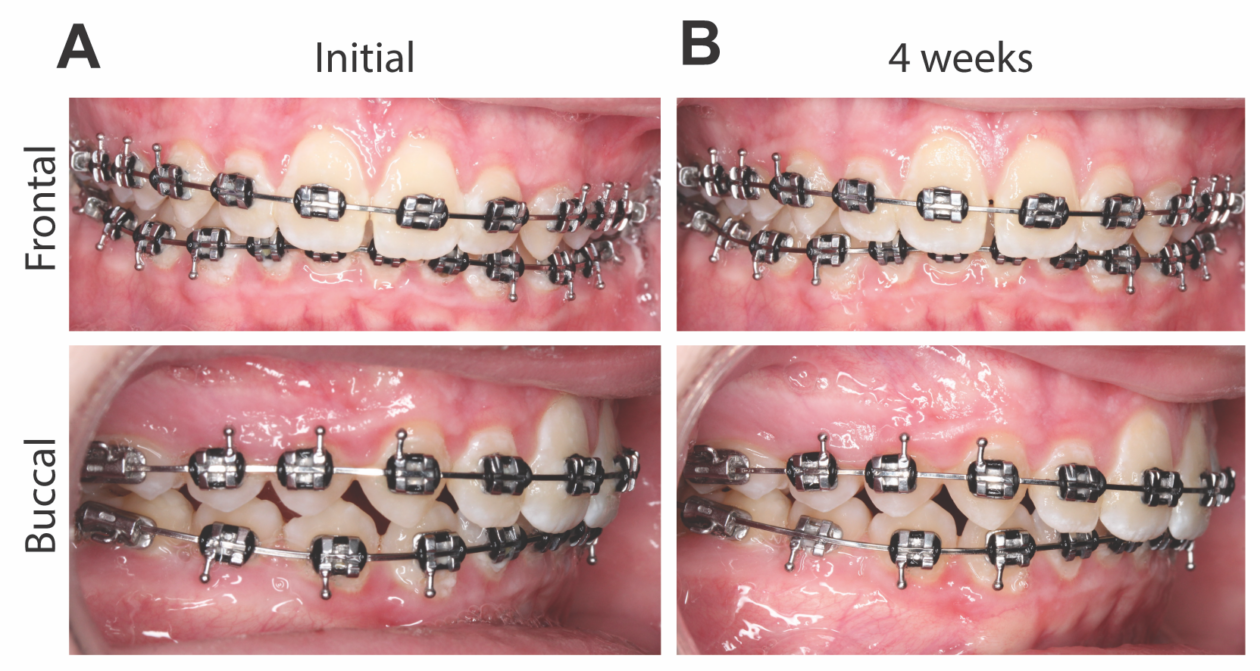
Seven subjects (2 female, 5 male) between the ages of 14-16 years old (mean age 14.9 years, standard deviation 0.67) were recruited in the study. The average initial plaque index across all subjects was 2.04 with a standard deviation of 0.75 (Fig. 2A), which equates to a moderate accumulation of soft deposition along the gingival pocket or tooth margin which can be observed with the naked eye. Moreover, the initial mean gingival index across subjects was 2.12 with a standard deviation 0.61, suggesting generalized redness, edema and bleeding upon probing (Fig. 2B). All patients began with a baseline OPI (orthodontic plaque index) of between 2-4, demonstrating that in each sextant, plaque was present on at least two to four surfaces on the orthodontic brackets (Fig. 2C). Representative images demonstrate visible marginal erythema and edema suggestive of gingivitis (Fig. 3A)
Qualitative surveys revealed that all participants rated their oral hygiene as a 3 out of 5, with zero representing very bad and five representing very good, and all participants rated the cleanliness of their teeth upon initiation in the study to be a 3 out of 5 after brushing, with zero representing very dirty and five representing very clean. Participants reported to be brushing 1-2 times a day for an average of 101 seconds (standard deviation of 71 seconds)
After four weeks of utilizing the O-R toothbrush with the Ultimate Clean brush head, coupled with the novel TC brush head, as part of the oral hygiene routine, patients returned and were evaluated for the same markers of oral hygiene. A notable decrease in all markers was observed with a mean decrease in the plaque index by 1.14 (standard deviation of 0.78) (Fig. 2A) and an average decrease of the gingival index by 1.01 (standard deviation of 0.70) (Fig. 2B). When assessing the orthodontic plaque index, a mean decrease of 1.79 was observed (standard deviation 0.89) (Fig. 2C) suggesting, on average that there was a 64% decrease of plaque around the orthodontic appliances during the four-week study period. Representative images highlight a visual reduction in marginal erythema and edema suggestive of decreased inflammation and improvements of gingivitis (Fig. 3B). When surveying participants, six of seven patients reported that they were more motivated to brush while using the OR power brush and all participants reported that they brushed longer, noticed in improvement in their oral hygiene and would recommend the power brush coupled with the novel brush head to a friend/family member.
Discussion
The utilization of an O-R electric brush with the Ultimate Clean brush head, coupled with the novel TC brush head, has demonstrated to dramatically improve the oral hygiene of patients who initially had poor oral hygiene and were undergoing orthodontic treatment. Patients not only had a decrease in plaque accumulation on the teeth and around the orthodontic appliances, as well as a decrease in gingivitis, but also reported to be more motivated to maintain proper oral hygiene.
As previously mentioned, studies have demonstrated that patients who have poor oral hygiene generally have longer treatment lengths, which can further worsen the patient’s oral hygiene condition.5, 6 Poor oral hygiene necessitates more frequent hygiene recalls and restorative appointments, which require wires to be removed and replaced, often costing the orthodontic practice and patient additional time and money. Moreover, this time-consuming process for the patient having to visit several dental professionals, often within the same day, also results in poor patient satisfaction through their orthodontic journey. Therefore, if we can improve the patient’s oral hygiene, it is not only advantageous for the patient, who now will have a healthier oral cavity, but also behooves the dental professional through a more enthusiastic patient, decreased office time/costs, and a better overall experience.
Conclusion
Utilizing an O-R power brush, coupled with a novel targeted clean brush head is an advantageous tool to incorporate in all orthodontic patients’ armamentarium. This combination has been shown to improve oral hygiene ratings in patients with poor oral hygiene in four weeks with a marked decrease in plaque and gingivitis. It is indeed difficult to properly remove plaque from around fixed orthodontic appliances using traditional manual toothbrushes, however with the advances in O-R technology as well as the optimization of brush heads, including the novel Targeted Clean, orthodontic patients are now equipped with the tools needed to maintain proper oral hygiene.
Acknowledgments
The study was supported by Procter & Gamble.
References
1. Grippaudo MM, Quinzi V, Manai A, et al. Orthodontic treatment need and timing: Assessment of evolutive malocclusion conditions and associated risk factors. Eur J Paediatr Dent. Sep 2020;21(3):203-208. doi:10.23804/ejpd.2020.21.03.09
2. Hamdan AM, Maxfield BJ, Tufekci E, Shroff B, Lindauer SJ. Preventing and treating white-spot lesions associated with orthodontic treatment: a survey of general dentists and orthodontists. J Am Dent Assoc. Jul 2012;143(7):777-83. doi:10.14219/jada.archive.2012.0267
3. Gontijo L, Cruz Rde A, Brandao PR. Dental enamel around fixed orthodontic appliances after fluoride varnish application. Braz Dent J. 2007;18(1):49-53. doi:10.1590/s0103-64402007000100011
4. Pari A, Ilango P, Subbareddy V, Katamreddy V, Parthasarthy H. Gingival diseases in childhood – a review. J Clin Diagn Res. Oct 2014;8(10):ZE01-4. doi:10.7860/JCDR/2014/9004.4957
5. Beckwith FR, Ackerman RJ, Jr., Cobb CM, Tira DE. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. Apr 1999;115(4):439-47. doi:10.1016/s0889-5406(99)70265-9
6. Skidmore KJ, Brook KJ, Thomson WM, Harding WJ. Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofacial Orthop. Feb 2006;129(2):230-8. doi:10.1016/j.ajodo.2005.10.003
7. Grender J, Adam R, Zou Y. The effects of oscillating-rotating electric toothbrushes on plaque and gingival health: A meta-analysis. Am J Dent. Feb 2020;33(1):3-11.
8. Yaacob M, Worthington HV, Deacon SA, et al. Powered versus manual toothbrushing for oral health. Cochrane Database Syst Rev. Jun 17 2014;(6):CD002281. doi:10.1002/14651858.CD002281.pub3
9. Clark-Perry D, Levin L. Systematic review and meta-analysis of randomized controlled studies comparing oscillating-rotating and other powered toothbrushes. J Am Dent Assoc. Apr 2020;151(4):265-275 e6. doi:10.1016/j.adaj.2019.12.012
10. Deacon SA, Glenny AM, Deery C, et al. Different powered toothbrushes for plaque control and gingival health. Cochrane Database Syst Rev. Dec 8 2010;(12):CD004971. doi:10.1002/14651858.CD004971.pub2
11. Erbe C, Klees V, Braunbeck F, et al. Comparative assessment of plaque removal and motivation between a manual toothbrush and an interactive power toothbrush in adolescents with fixed orthodontic appliances: A single-center, examiner-blind randomized controlled trial. Am J Orthod Dentofacial Orthop. Apr 2019;155(4):462-472. doi:10.1016/j.ajodo.2018.12.013
12. Erbe C, Klees V, Ferrari-Peron P, et al. A comparative assessment of plaque removal and toothbrushing compliance between a manual and an interactive power toothbrush among adolescents: a single-center, single-blind randomized controlled trial. BMC Oral Health. Aug 3 2018;18(1):130. doi:10.1186/s12903-018-0588-1
13. Erbe C, Jacobs C, Klukowska M, Timm H, Grender J, Wehrbein H. A randomized clinical trial to evaluate the plaque removal efficacy of an oscillating-rotating toothbrush versus a sonic toothbrush in orthodontic patients using digital imaging analysis of the anterior dentition. Angle Orthod. May 2019;89(3):385-390. doi:10.2319/080317-520.1
14. Adam R, Ram Goyal C, Qaqish J, Grender J. Evaluation of an oscillating-rotating toothbrush with micro-vibrations versus a sonic toothbrush for the reduction of plaque and gingivitis: results from a randomized controlled trial. Int Dent J. Apr 2020;70 Suppl 1:S16-S21. doi:10.1111/idj.12569
15. Grender J, Ram Goyal C, Qaqish J, Adam R. An 8-week randomized controlled trial comparing the effect of a novel oscillating-rotating toothbrush versus a manual toothbrush on plaque and gingivitis. Int Dent J. Apr 2020;70 Suppl 1:S7-S15. doi:10.1111/idj.12571
16. Beberhold K, Sachse-Kulp A, Schwestka-Polly R, Hornecker E, Ziebolz D. The Orthodontic Plaque Index: an oral hygiene index for patients with multibracket appliances. Orthodontics (Chic). 2012;13(1):94-9.


